ONC adapted this glossary from the one compiled by the Center for Healthcare Quality and Payment Reform. Use it throughout your health IT journey to create a foundation for a common language for developing and discussing payment reform with all stakeholders.
A
Accountable Care Organization (ACO). An Accountable Care Organization is a group of clinicians who have organized themselves in a way that enables them to take accountability for the overall quality of care and the total cost to payers of all or most of the healthcare services needed by a group of patients over a period of time. In the Affordable Care Act, Congress authorized the use of different methods of paying for services to Medicare beneficiaries if the clinicians are part of an Accountable Care Organization that meets specific eligibility criteria established in the statute and in regulations promulgated by the Centers for Medicare and Medicaid Services (CMS). However, the term Accountable Care Organization is also used to describe clinician organizations that may not meet all of the standards established in the Medicare Shared Savings program but are measuring and managing the cost and quality of services for their patients.
An Accountable Care Organization is not a payment model — it is an organizational structure designed to deliver care in a different way. Although CMS is paying clinicians that meet its ACOs standards using a shared savings payment model, the Affordable Care Act authorized the use of other payment models for ACOs in the Medicare program, including partial capitation. A number of clinicians who have defined themselves as an Accountable Care Organization are participating in payment contracts with commercial health insurance plans, Medicaid programs, etc. that use payment models different from the payment model used in the Medicare Shared Savings Program. Moreover, clinicians do not need to form an ACO in order to participate in a shared savings payment model, since many payers, including CMS, are using shared savings payment models to pay individual physician practices and hospitals that are not part of an Accountable Care Organization.
While CMS has defined an Accountable Care Organization as a group of clinicians that includes primary care physicians and that takes accountability for the costs of all services associated with the patients attributed to those primary care physicians, the term Accountable Care Organization is also used to describe a group of specialists who take accountability for all of the costs related to a particular health condition, such as cancer.
Next Generation ACO. The Next Generation ACO Program is a demonstration program announced by the Center for Medicare and Medicaid Innovation in 2015. It offers multiple payment options, including a capitation payment model, and it requires clinicians to accept virtually full performance risk and some insurance risk for the population of Medicare beneficiaries assigned to the ACO.
Pioneer ACO. A Pioneer ACO is a clinician organization participating in a special demonstration program with the Center for Medicare and Medicaid Innovation using a shared savings payment model with different rules than those that apply to clinician organizations participating as ACOs in the Medicare Shared Savings Program.
Track 1 ACO. In the Medicare Shared Savings Program, a “Track 1 ACO” is an Accountable Care Organization that is eligible for a shared savings payment if savings are achieved, but the ACO is not liable to make payments to CMS if spending increases (i.e., Track 1 is an “upside only” shared savings model).
Track 2 ACO. In the Medicare Shared Savings Program, a “Track 2 ACO” is an Accountable Care Organization that is eligible for a shared savings payment if savings are achieved, but the ACO is also liable to make payments to CMS if spending increases (i.e., Track 2 is a “shared risk” payment model).
Track 3 ACO. In the Medicare Shared Savings Program, a “Track 3 ACO” is an Accountable Care Organization that is eligible for a shared savings payment if savings are achieved and is liable to make payments to CMS if spending increases, but the ACO receives a greater share of savings and is liable for larger payments to CMS than a Track 2 ACO.
ACO vs. HMO vs. PPO. There are a number of important similarities and differences between ACOs, HMOs (Health Maintenance Organizations), and PPOs (Preferred Clinician Organizations):
- An ACO is generally based on a self-defined network of clinicians, whereas in most HMOs and PPOs, the network is defined by a health plan.
- In the Medicare Shared Savings Program and most commercial ACOs that are part of PPO health plans, an ACO cannot limit a patient’s ability to use clinicians that are not part of the ACO, whereas the primary care clinicians in an HMO typically have the ability to limit which services a patient can receive and from which clinicians they can receive approved services. In the Medicare Shared Savings Program, a Medicare beneficiary remains able to use any Medicare clinician, and in most commercial ACO programs, a commercially- insured patient can continue to use any clinician in the network of clinicians that is under contract to the payer.
- In an ACO that is paid through shared saving programs, there is no change to the underlying fee-for-service payment structure for the clinicians in the ACO. In contrast, in many HMOs, a clinician group receives a capitation payment that it can use to pay its physicians and other clinicians in different ways.
Accountable Payment Model. An Accountable Payment Model is a generic term describing a payment model in which an accountable clinician takes responsibility for achieving specific performance levels on quality and cost measures and receives a payment designed to support the services and activities needed to achieve those performance levels. See Payment Model and Accountable Clinician.
Accountable Clinician. In any payment model, there needs to be an accountable clinician who accepts responsibility for ensuring that a payment is used to produce the results that are expected, whether that be the delivery of one or more specific services to the patient or achieving specific outcomes for the patient. In a traditional fee-for-service payment model, it is straightforward to identify the accountable clinician because it is the individual or clinician organization that bills for payment for a particular service. However, in shared savings payment models, multi-clinician bundled payment models, and global payment models, where a patient receives services from multiple clinicians, a method is generally needed for determining which clinician is the accountable clinician. This can be done either by having the clinician agree to accept accountability before the relevant services are to be delivered, or by using a retrospective attribution methodology to designate the accountable clinician.
ACE Demonstration. See Acute Care Episode Demonstration.
Achievement. In a payment model where the amount of payment is based on performance on one or more measures of quality or spending, “achievement” is used to refer to the clinician’s level of performance compared to a benchmark that is established in some way. In contrast, “improvement” is a measure of how the clinician’s own level of performance has changed over time. Since a clinician may have improved its performance but failed to meet an achievement threshold, many pay-for-performance systems are based on both achievement and improvement.
Achievement Threshold. In a pay-for-performance system, an achievement threshold is a level of achievement that must be reached in order to qualify for a payment or an adjustment in payment.
ACG. See Adjusted Clinical Groups.
ACO. See Accountable Care Organization.
Actuarially Equivalent. Two health insurance plans or bundled payments are said to be actuarially equivalent if it is estimated that the total spending on the services that the insured members receive under the two plans or payments will be the same.
Acute Care Episode Demonstration. The Acute Care Episode (ACE) Demonstration was a Medicare demonstration project in which several hospitals and their affiliated physicians received bundled payments for cardiovascular and orthopedic procedures.
Adjudication. Adjudication is the process through which a payer determines that a claim from a clinician for delivery of healthcare services should be paid and the allowed amount for the claim. See also Allowed Amount.
Adjusted Clinical Groups (ACGs). Adjusted Clinical Groups (ACG) is a risk adjustment system developed by Johns Hopkins University that uses information on the duration, severity, diagnostic certainty, and origin of a patient’s diagnoses to categorize each of the patient’s health problems into one of 32 diagnosis clusters. Then, based on the patient’s age, sex, and the diagnosis clusters applicable to them, the patient is assigned to one of 93 different ACG categories.
Administrative Services Only (ASO). In an Administrative Services Only contract, an insurance company or Third-Party Administrator (TPA) agrees to receive and pay claims on behalf of a self-funded employer or other self-insured purchaser, but the ASO entity does not take any direct risk related to the cost of those claims.
Alignment. In the context of payment models, the word “alignment” is being used in three different ways:
- Alignment of a payer’s payment models for multiple clinicians. In this context, “alignment” means that a payer pays two different clinicians in ways that encourage them to work together toward the same outcomes. For example, hospital and physician payment models are said to be “aligned” if they reward both the hospital and the physician for improvements in the same quality measure.
- Alignment of the payment models used for a single clinician by multiple payers. In this context, “alignment” means that two different payers are using payment models that are structured in similar ways. For example, two different pay-for-performance systems are said to be aligned if they use the same quality measures to adjust payments.
- Alignment of patients to a particular clinician. In some of its demonstration programs, CMS has described the process of having beneficiaries attributed to a clinician as “aligning” the beneficiaries; i.e., in this context, “alignment” is a synonym for “attribution.”
Allowed Amount. The allowed amount is the total payment that a clinician is eligible to receive for a particular service delivered to a patient insured by a payer. The clinician is generally responsible for collecting the patient’s cost-sharing, so the payer pays the clinician the allowed amount less than the required patient cost-sharing.
All Payer Claims Database (APCD). An All Payer Claims Database is a database containing information from the claims received or paid by all or most of the third-party payers who pay for claims for services rendered to patients living in a geographic area, such as a state or metropolitan area. A number of state governments have established All Payer Claims Databases and require health insurance plans to submit information from the claims they pay for residents of the state.
Alternative Payment Entity. The Medicare Access and Chip Reauthorization Act (MACRA) defines an Alternative Payment Entity as an organization that (1) participates in an Alternative Payment Model that meets the requirements of the law and also (2) either (a) bears “financial risk for monetary losses under such alternative payment model that are in excess of a nominal amount,” or (b) is a medical home expanded under the powers of the Center for Medicare and Medicaid Innovation. An Alternative Payment Entity could be an existing clinician organization that accepts payment under fee for service or other standard payment models, but it could also be an organization that is specifically created to accept payments under an Alternative Payment Model and then allocates those payments to individual clinicians.
Alternative Payment Model (APM). The term “alternative payment model” has generally been used to describe a method of paying for services in which clinicians can voluntarily choose to participate that is different from the standard payment method used to pay those clinicians. (See the definition of Payment Model for a description of the elements of a payment model that can be used to define how an alternative payment model differs from existing payment models.)
In the Medicare Access and Chip Reauthorization Act (MACRA), Congress authorized higher fee-for-service payments to physicians who receive a specific proportion of their revenues, or who are paid for a specific proportion of their patients, through an Alternative Payment Model that meets criteria established in the law and in regulations to be promulgated by CMS.
MACRA establishes two slightly different sets of criteria for defining an Alternative Payment Model, one for payments in the traditional Medicare program and one for payments from other payers.
For Medicare payments, an Alternative Payment Model must be either:
- One of the innovative payment models described in Section 1115A of the Social Security Act establishing the Center for Medicare and Medicaid Innovation (see Center for Medicare and Medicaid Innovation for a description of the models in Section 1115A);
- The Medicare Shared Savings Program;
- A demonstration under the Healthcare Quality Demonstration Program; or
- A demonstration program required under federal law.
In addition, the Alternative Payment Model must:
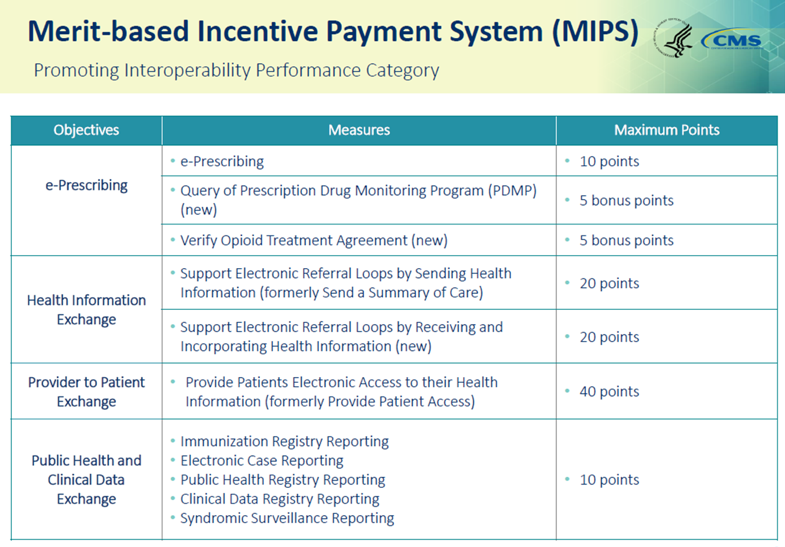
- require participants to use certified EHR technology;
- base payments on quality measures comparable to those used in the Merit-Based Incentive Payment System (MIPS); and
- make payments through an Alternative Payment Entity that either (1) bears financial risk for monetary losses under the Alternative Payment Model that are in excess of a nominal amount, or (2) is a medical home tested and expanded by the Center for Medicare and Medicaid Innovation.
For payments from other payers, the Alternative Payment Model must:
- use quality measures comparable to those used by Medicare in the Merit-Based Incentive Payment System (MIPS);
- use certified EHR technology;
- make payments through an entity that “bears more than nominal financial risk if actual aggregate expenditures exceeds expected aggregate expenditures” or, for Medicaid beneficiaries, is a medical home similar to medical homes tested and found to be effective by the Center for Medicare and Medicaid Innovation.
Ambulatory Patient Groups (APGs). Ambulatory Patient Groups (APGs) is a system of classifying patients into categories based on their expected relative use of outpatient hospital services and other ambulatory care services that was developed and is maintained by 3M Information Systems. It was originally designed for use as part of the Medicare Outpatient Prospective Payment System, but it was not implemented as part of the OPPS (Ambulatory Payment Classifications were used instead). APGs are similar to DRGs but are designed to risk adjust payments for services delivered in outpatient settings rather than inpatient settings.
Ambulatory Payment Classifications (APCs). Ambulatory Payment Classifications (APCs) are used in the Medicare Outpatient Prospective Payment System (OPPS) to define the amounts Medicare will pay for services delivered in outpatient hospital departments. They provide a mechanism for partial bundling of individual hospital outpatient services. APCs are not a riskadjustment system, since they do not provide a way of differentiating spending or performance levels based on patient characteristics independent of the services actually delivered. See Outpatient Prospective Payment System for more information.
Alternative Quality Contract (AQC). The Alternative Quality Contract (AQC) is a risk-adjusted global budget payment model used by Blue Cross Blue Shield of Massachusetts.
Ancillary Services. The term ancillary services is generally used to describe three different types of services:
- laboratory tests and imaging that support accurate diagnosis of patients, but do not have a direct therapeutic value in addressing a patient’s health condition.
- services such as physical therapy, nutrition counseling, dispensing of medications, etc. that have therapeutic value but are not delivered by a physician.
- services such as home care aides, assisted living facilities, hospice services, etc. that assist patients in managing activities of daily living or improve their quality of life but do not have direct therapeutic value in treating a health condition. (Some of these services are sometimes referred to as “custodial” services.)
The federal Stark Law prohibits physicians from referring patients for services, including ancillary services, delivered by clinicians in which the physician has a financial interest. An exception is ancillary services delivered in the physician’s office that meet the criteria for the In-Office Ancillary Services Exemption.
Anti-Kickback. The federal Anti-Kickback statute makes it a felony for any person to knowingly and willingly offer, solicit, or receive any remuneration for either referring a patient for an item or service, or for arranging or recommending an item or service, paid in whole or in part under a federal healthcare program. Many states have also enacted anti-kickback statutes or regulations. The federal Anti-Kickback statute and state anti-kickback laws can make it illegal to create payment models in which physicians are rewarded for following specific guidelines regarding the use of particular drugs or devices that have lower costs and higher quality.
The Office of Inspector General at the U.S. Department of Health and Human Services (OIG), which is responsible for interpreting the federal Anti-Kickback law and is one of the agencies responsible for enforcing it, can issue advisory opinions upon request concerning the applicability of the federal Anti-Kickback statute to specific arrangements. The OIG has created some “safe harbors” that protect certain types of arrangements from liability under the federal Anti-Kickback statute.
Antitrust. Federal and state antitrust laws are designed to prohibit payers and clinicians from jointly acting in anti-competitive ways, such as payers colluding to reduce clinician payments or clinicians colluding to raise prices. Antitrust laws can also create barriers to the kinds of cooperation or coordination among payers and clinicians that have the potential to improve quality of care or reduce the cost of care. For example, efforts to reach agreement among multiple health insurance plans to use a new approach to payment (i.e., alignment of payment models) can raise concerns about antitrust violations, even if there is no discussion or agreement on the actual payment levels. Multiple independent clinicians who want to work together as an Accountable Care Organization or Clinically Integrated Network may fear antitrust action if they attempt to negotiate a joint contract with payers, even if their goal is to create a more efficient and effective method of delivering care.
The Federal Trade Commission (FTC) and the U.S. Department of Justice (DOJ) have issued joint statements indicating that they are not likely to challenge joint conduct of physicians in a physician network joint venture or participants in a multi-clinician network if those physicians or participants share substantial financial risk, e.g., through a global payment arrangement such as capitation, or if they are clinically integrated.
States can protect healthcare payers and clinicians from antitrust liability under the “state action” doctrine of antitrust law if the state (1) has a clearly articulated state policy supporting the need for common approaches, and (2) engages in active supervision of the activities that might otherwise cause antitrust concerns.
APCD. See All Payer Claims Database.
APM. See Alternative Payment Model.
Appropriate Use Criteria (AUC). Appropriate use criteria are guidelines established by a medical society or other organization to help physicians or other clinicians to select the services that are appropriate for a particular patient. In general, the term “appropriate” is used to mean that the benefits to the patient are much greater than the risks, but the tradeoff between benefits and risks is inherently a subjective decision. Some payment models require clinicians to follow appropriate use criteria in order to be paid, or pay higher amounts if the criteria are followed. See also Clinical Pathway.
APC. See Ambulatory Payment Classification.
APG. See Ambulatory Patient Group.
APR-DRG (All Patient-Refined Diagnosis Related Group). APR-DRGs are a version of DRGs developed and maintained by 3M Information Systems. They are applicable to a broader range of patients than the version of DRGs (called MS-DRGs) used in the Medicare Inpatient Prospective Payment System.
ASP. See Average Sales Price.
Assignment (for Physicians). A physician “accepts assignment” in the Medicare program by agreeing to accept the Medicare Physician Fee Schedule payment (80% from Medicare and 20% cost-sharing from the patient) as payment in full for a service to a Medicare beneficiary. A physician who accepts assignment for all services is described as a “participating physician.” For more information, see Participating Physician.
Assignment (for Patients). In many HMO health plans, a patient is assigned to a primary care physician if the patient does not choose a physician or other clinician as their designated primary care clinician. In some shared savings and other payment models, the word “assignment” is used as a synonym for attribution.
Attachment Point. An attachment point is a dollar amount established in a stop-loss policy purchased by a clinician or health insurance plan from a reinsurer, such that when the total amount of costs or claims payments incurred by the clinician or health plan reaches the attachment point, the reinsurer pays all or part of the amount of costs or claims above the attachment point. For more information, see Stop-Loss.
Attestation (by Clinician). A statement by a healthcare clinician that a task has been performed, a goal has been achieved, or a criterion has been met. For example, in pay for performance programs, if it is difficult for a payer to independently measure whether a clinician is carrying out a particular activity, the clinician may be asked to attest that the activity is being performed.
Attestation (by Patient). In order for a payer to know which clinician will be accountable for quality or costs under a payment model, a patient may be asked to attest that the clinician is managing the patient’s care under the payment model. For alternative methods of identifying accountable clinicians, see Assignment and Attribution.
Attribution. Attribution is a process for determining which healthcare clinician or clinicians should be held responsible for one or more specific aspects of the cost or quality of a patient’s care in the absence of an explicit signal from the patient or a particular clinician that the clinician will be responsible. For example, when one of a health plan’s members is admitted to the hospital, the health plan may “attribute” responsibility for that admission to a primary care physician that the member had seen during the prior year, even if the physician did not order the admission, did not provide any services during the admission, was not aware that the admission occurred, and did not explicitly accept responsibility for providing services to the patient that could have avoided the admission.
NOTE: CMS has used the word “assignment” to describe its attribution process in the Medicare Shared Savings Program; however, this is confusing because “assignment” is commonly associated with a prospective process in which the patient is notified of their assignment. CMS has also used the term “alignment” to describe the Medicare beneficiaries who have been attributed to an ACO or other clinician.
Attribution is not needed for issues related directly to a specific service that a specific clinician delivered to a patient, because it is obvious which clinician delivered that service. Attribution is also not needed if a clinician has been assigned in advance the responsibility for that aspect of cost or quality for that patient. For example, if a health insurance plan requires a patient to designate a primary care physician, then the designated PCP can be held responsible for various aspects of the cost and quality of the patient’s care, and there is no need for an attribution methodology. (See also Assignment and Attestation.) The need for attribution arises when (a) there is a desire to hold a clinician responsible for (i) services delivered by other clinicians, (ii) for a patient’s failure to obtain needed services, or (iii) for potentially preventable problems or complications that a patient experienced, and (b) there are multiple clinicians who could potentially be held responsible and none have been assigned responsibility in advance. An attribution methodology identifies which, if any, clinicians could potentially be assigned responsibility and then chooses one or more of the clinicians based on an algorithm or set of rules.
An attribution methodology can be designed to choose only a single clinician or it can allow more than one clinician to be assigned responsibility for the same event or outcome. If more than one clinician is assigned responsibility, the methodology may or may not define an allocation of responsibility among the clinicians (i.e., two clinicians could both be assigned 100% responsibility for the same event or outcome, or that responsibility could be allocated between them in some proportion).
An attribution methodology generally involves a number of inherently arbitrary decisions about the variables and calculations used in the methodology, such as the clinicians who are eligible for attribution, the measure used for attribution, the threshold the measure must reach in order for a patient to be attributed based on the measure, the look-back period, what tiebreakers will be used, and how often attribution is done. Studies have shown that the results of the attribution process can differ dramatically depending on the methodology used. Moreover, most attribution methodologies cannot attribute some patients, events, or outcomes to any clinician, in which case those patients, events, or outcomes are “unattributed” and no clinician is held accountable for them.
Attribution is inherently a retrospective process – the attribution methodology looks backward in time to determine which clinicians were involved with a patient’s care and could potentially have influenced the aspect of cost or quality in question and then the methodology chooses one or more of those clinicians to hold accountable for a performance measure. Despite the confusing name, even what is referred to as “prospective attribution” is still inherently a retrospective process.
Prospective Attribution. Under common retrospective attribution methodologies, a clinician does not know which patients the clinician is being held accountable for until after the care has already been delivered. A partial solution to this is what is called “prospective attribution.” It is still a retrospective calculation, i.e., it is based on where a patient received services during a time period prior to when the attribution is determined, rather than where the patient intends to obtain services in the future, but it is prospective in the sense that the attribution is made prior to the beginning of the time period in which a clinician’s performance is being measured. However, a patient who had been receiving services from one clinician during the period of time on which the attribution calculation is based may decide to use a different clinician after the attribution calculation is completed; this means that some patients who are attributed to a clinician under prospective attribution will be receiving their care from some other clinician during the performance period, and patients who began receiving care from a clinician during the performance period will not have been attributed to that clinician.
Two-Step Attribution. A two-step attribution methodology first attempts to attribute individuals to a clinician using one formula, and if no clinician meets the criteria for attribution, a second formula is used. For example, in the Medicare Shared Savings Program, the first step is to try to attribute a beneficiary to a primary care physician, but if the beneficiary has not received any primary care services from a primary care physician, the attribution methodology then looks for specialists who have delivered primary care services to the patient.
AUC. See Appropriate Use Criteria.
Average Sales Price. In the buy and bill system used by Medicare and many commercial payers to pay physicians and hospitals for drugs administered to patients in physician offices or infusion centers, the payment to the clinician for the drug is based on the “Average Sales Price” (ASP) of the drug. Each drug manufacturer reports the average amount it was paid for each of its drugs on a quarterly basis to enable CMS to calculate the ASP. The amount paid to clinicians for use of a drug is based on the ASP for the drug two quarters earlier plus a small additional percentage of the ASP (e.g., the total payment to the clinician for the drug is 106% of ASP). As a result, the payment from Medicare to a clinician for administering a drug can be higher or lower than the amount the clinician paid to acquire that drug from the manufacturer or a wholesaler, and the difference will vary from drug to drug, from quarter to quarter, and from clinician to clinician.
Back to top
B
Balance Billing. Balance billing is a form of cost-sharing. If the combination of the payment from a payer for a service and the patient’s cost-sharing amount required by the payer is less than the amount the clinician charges for a service, balance billing is a process whereby the clinician requires the patient (or some other payer) to pay for all or part of the remainder of the clinician’s charge. Many payment contracts prohibit balance billing and require a clinician to accept the payer’s payment and the patient’s cost-sharing amount as payment in full for a service.
Balance billing is an alternative to co-payments, coinsurance, and deductibles for having patients share the cost of healthcare services; under balance billing, the patient pays the “last dollar” of costs (i.e., the difference between the amounts two clinicians charge) rather than the “first dollar” of costs; this gives the patient a stronger incentive to choose lower-priced clinicians and services than under other forms of cost-sharing. Balance billing is also an integral part of a reference price benefit structure, where the payer agrees to pay up to the reference price for a particular service and then the patient pays the remainder of the clinician’s charge. However, balance billing could result in very high prices if there is only one clinician available to deliver a service a patient needs unless there is way to limit the amount the clinician can charge.
Baseline. A baseline is a clinician’s performance level on a spending or quality measure during a period of time (a baseline period) prior to a performance period. A clinician’s payment may be based in part on a comparison of its performance during the performance period relative to the baseline.
Baseline Period. A baseline period is a period of time in which a clinician’s baseline performance is measured.
BPCI. See Bundled Payments for Care Improvement.
Benchmark. A benchmark is a particular level on a measure of spending or quality that a clinician must achieve in order to qualify for a payment or a payment adjustment. In addition, the payment adjustment may be proportional to the amount of difference between the clinician’s performance level and the benchmark level. For example, in many shared savings payment models, the spending for a clinician’s patients must be below a benchmark spending level and multiple quality measures must be above benchmark quality levels in order for the clinician to qualify for a shared savings payment, and then the amount of the shared savings payment is proportional to the amount of savings (as determined by the difference between the clinician’s spending and the benchmark level for spending ) and the level of quality (as determined by the difference between the clinician’s quality scores and the benchmark levels for quality).
A benchmark can be determined in many ways. Most approaches fall into one of the following two categories:
- Trending the clinician’s baseline performance forward to the performance period. In this approach, the clinician’s performance is calculated during a baseline period that precedes the performance period. Then a method is used to adjust that performance level in some way to serve as a benchmark during the performance period. For example, the clinician’s spending level during the year preceding the performance year might be trended forward using a measure of inflation (such as the Medicare Economic Index) to estimate what spending would be in the performance year with no change in service delivery. This trended spending level serves as the benchmark, and if the actual spending is below that level, the clinician is determined to have achieved savings.
- Calculating the distribution of performance for other clinicians during the performance period. In this approach, the same measure is computed for all other clinicians during the same period as the clinician’s performance is being measured, and then a particular point on the distribution is chosen as the benchmark. For example, the benchmark might be set at the median or 75th percentile of the performance of other clinicians on the spending or quality measure. See Tournament Pay for Performance for additional information.
Benefit Design. In a health insurance plan, the benefit design is a set of rules that describe which types of healthcare services will be covered by the plan, the clinicians from which a member of the plan can receive a covered service, the cost-sharing amounts that a member of the plan will be responsible to pay when receiving a service, and any other requirements or restrictions on how or when the plan member can receive covered healthcare services. See also Value-Based Insurance Design.
Billing Code. A billing code is a numeric code identifying a service, procedure, bundle of services, episode of care, patient condition, or type of patient for which a clinician is requesting payment under a fee-for-service, bundled payment, episode-of-care payment, or condition-based payment model. Although traditional billing codes have been associated with delivery of a specific service (e.g., knee replacement surgery), billing codes can also be used to request payment for a procedural bundle or episode of care (e.g., all services associated with knee replacement surgery, including post-acute care and treatment of complications) or to request payment for care of a particular condition (e.g., treatment of knee osteoarthritis, regardless of the specific treatment used).
Budget-Neutral. A change in a payment system is said to be “budget neutral” if (1) the additional spending on one set of services that is estimated to result from increases in payments or the volume of services is less than or equal to (2) the reduction in spending that is estimated to result from lower payments for other services or lower volumes of other services.
Bundled Payment. A payment is described as “bundled” when it covers multiple healthcare services, particularly if those services had previously been paid for separately. Bundling is a very generic term and it can apply to many different combinations of services, so the mere fact that a payment is “bundled” does not communicate very much. For example, a bundled payment can involve just one clinician or many clinicians and it can involve two services or dozens of services. (Many current fee-for-service payments are already “bundled;” see Bundled Payment vs. Fee-for-Service). At one extreme, bundling two services that a patient always receives in the same combination from the same clinician may accomplish little more than to simplify billing and payment slightly (since the clinician bills for one combined service rather than two and the patient has one cost-sharing payment rather than two); at the other extreme, a “global payment” that includes all services from all clinicians in a single bundle can potentially lead to dramatic changes in what services are delivered and who delivers them.
Depending on how they are structured, bundled payments can potentially help achieve one or more of four distinct goals:
- Bundling multiple services delivered by the same clinician into a single payment can encourage greater efficiency in the delivery of care, since the clinician will no longer be paid more for delivering more of the services covered by the bundle. This type of bundle can also allow the clinician more flexibility to deliver innovative services if the bundled payment no longer limits the clinician to delivering services that meet the narrow definitions of the individual services that were previously paid for separately.
- Bundling services delivered by two or more clinicians into a single payment can encourage greater coordination among those clinicians, since the clinicians have to agree on which services will be delivered and how the payment should be divided among them. This type of bundle can also encourage greater efficiency if one or more of the clinicians is delivering services that are not essential to a good outcome.
- Bundling a treatment with any services required to address complications of the treatment can encourage higher quality of care, since the clinicians will not receive additional compensation for costs incurred in treating complications. Such a bundle is a way of implementing a Warrantied Payment.
- Bundling all services associated with a particular procedure or treatment of a particular condition into a single payment can provide greater predictability for purchasers and patients regarding their cost for delivery of that procedure or treatment of that condition and improve their ability to compare costs and value between different clinicians that deliver the same procedure or treat the same condition.
The more services that are bundled into a single payment and the more different kinds of patients for whom the bundled payment is made, the greater the need there will be for risk adjustment as part of the bundled payment, since different patients may need different combinations of services for reasons beyond the control of the clinician.
In addition, a bundled payment involving services delivered by two or more independent clinicians can cause problems under the federal Stark Law and other federal Fraud and Abuse laws unless waivers are granted in law or by enforcement agencies.
Partial Bundle. A partial bundle is a bundled payment that includes some, but not all, services that are related to delivery of a particular treatment or management of a particular health condition. For example, payments to hospitals under the Medicare Inpatient Prospective Payment System are increasingly seen as partial bundles; although they bundle together all of the services delivered by the hospital as part of a patient’s inpatient stay, they do not bundle the physician services that occurred at the same time as the hospital services and they do not include any post-acute care services. Global surgical fees paid to surgeons are also partial bundles, since they bundle post-surgery visits to patients made by the surgeon into a single payment, but they do not bundle visits made by other physicians.
Bundled Payment vs. Episode Payment. An episode payment is generally a bundled payment, since typically multiple services are delivered as part of a single episode of care. However, a bundled payment need not be an episode payment; the bundle could involve only a portion of an episode of care (or it could involve multiple episodes of care). For example, an episode of care for surgery performed in the hospital is typically viewed as including both the services provided during the hospital stay as well as any services related to the surgery that occur for a period of time after discharge from the hospital. However, a bundled payment could be defined as all of the services that occur during the hospital stay without including services that occur after discharge in the bundle (as was done in the Medicare Acute Care Episode demonstration), and a bundled payment can be defined as all of the post-acute care services that occur after discharge without including the initial hospitalization in the bundle (as is being done in Model 3 of the Bundled Payments for Care Improvement demonstration).
Bundled Payment vs. Shared Savings. In a bundled payment model, a single new payment replaces two or more separate payments and a specific price is set for the bundle. The clinician or clinicians accepting the bundle know in advance how much money they will receive for delivering services within the bundle, they have the flexibility to determine which and how many services are to be delivered within the payment, including (depending on how the bundle is defined) the flexibility to deliver different types of services in different ways, and they are accountable for holding the costs of the services actually delivered below the price of the bundle. In contrast, in a shared savings model focused on the same services, the clinician(s) are initially paid for services the same way as they are today, and so the clinicians may not be paid at all for delivering a different service or delivering a service in a different way, causing short-term losses. In addition, whereas the price of a bundle can be set in advance based on the expected cost to deliver appropriate services and the bundle price for some patients could be higher than current spending if outcomes are better, shared savings payments are only made if spending is lower, even if outcomes can be improved with no change in spending. However, a bundled payment requires knowing enough about how care can be delivered to determine whether a bundled price will be adequate, whereas in a shared savings model, a clinician can be assured of the same revenues if care remains the same.
Bundled Payment vs. Fee for Service Payment. Contrary to popular belief, bundled payments are not a radical change from fee-for-service payments. In fact, many payments in typical fee-for-service systems are already bundled to some extent. For example, the payment that is typically made for a physician office visit (an “evaluation and management” service) is intended to cover multiple tasks the physician performs before the visit and after the visit as well as what is done during the visit, and the time during the visit is intended to cover multiple activities. The fee-for-service payment made to surgeons for surgery is typically a “global fee” which bundles together the surgery itself and the separate visits the surgeon has with the patient before and after the surgery. If the surgeon accepts the global fee, the surgeon is not permitted to bill separately for office visits with the patients to follow up on the surgery and therefore does not get paid differently based on how many post-surgical visits he or she has with the patient.
Bundled Payments for Care Improvement (BPCI). Bundled Payments for Care Improvement (BPCI) is a demonstration project operated by the Center for Medicare and Medicaid Innovation (CMMI) that enables a clinician or group of clinicians to receive a bundled payment for a range of different procedures and conditions with the bundled payments structured in one of four different ways. All of the BPCI bundled payments are triggered by a hospitalization. The four different models are:
BPCI Model 1. In Model 1 of the Bundled Payments for Care Improvement demonstration, if a hospital accepts a discounted payment under the Inpatient Prospective Payment System, the hospital is permitted to make gaining-sharing payments to physicians based on internal cost savings the hospital generates. There is no actual change in the way the clinicians are paid by Medicare under this model, merely a change in the amount of payment to the hospital.
BPCI Model 2. In Model 2 of the Bundled Payments for Care Improvement demonstration, a budget is defined for a clinical condition, with the budget covering an episode of care that includes the acute care hospital stay, the physician services, and any post-acute care services or hospital readmissions that occur 30-90 days after discharge from the hospital. If the total Medicare payments for services during the episode are below the budget, the entity that is accountable in the demonstration receives the difference, and if the total payments are higher than the budget, the entity is responsible for paying Medicare for the difference. An entity participating in the demonstration can do so for one or more of 48 different clinical conditions. BPCI Model 2 uses a retrospective reconciliation process to ensure spending matches the budget; there is no change in the way the clinicians are initially paid for their services.
BPCI Model 3. In Model 3 of the Bundled Payments for Care Improvement demonstration, a budget is defined for a clinical condition, with the budget covering an episode of care that begins after the patient is discharged from the hospital and includes any post-acute care services or hospital readmissions that occur 30-90 days after discharge from the hospital. If the total Medicare payments for services during the episode are below the budget, the entity that is accountable in the demonstration receives the difference, and if the total payments are higher than the budget, the entity is responsible for paying Medicare for the difference. An entity participating in the demonstration can do so for one or more of 48 different clinical conditions. BPCI Model 3 uses a retrospective reconciliation process to ensure spending matches the budget; there is no change in the way the clinicians are initially paid for their services.
BPCI Model 4. In Model 4 of the Bundled Payments for Care Improvement demonstration, a single bundled payment is made to a hospital to cover the hospital services and all physician services during the hospital stay and any related readmissions for 30 days after hospital discharge (but not post-acute care services, which continue to be paid separately). Bundled payments can be defined for one or more of 48 different clinical conditions. BPCI Model 4 is a prospective bundled payment which replaces the current payments to the hospital under IPPS and physician payments under PFS.
Bundled Payment Discount. A bundled payment discount is the amount by which a bundled payment is lower than the estimated payments that would have been made under the existing payment system. For example, if a bundled payment is being made to a hospital and surgeon for delivery of surgical services in the hospital, the amount of the bundled payment might be set at 5% (the bundled payment discount) below the sum of the hospital payment under the Inpatient Prospective Payment System and the physician payment under the Physician Fee Schedule.
Buy-and-Bill. Buy-and-bill is a method of paying physicians and hospitals for pharmaceuticals administered to patients in an outpatient setting. It is called buy-and-bill because the clinician buys a drug from a manufacturer or wholesaler using the clinician’s own resources and then after the clinician administers the drug to a patient, the clinician bills the payer for a payment amount that is established in a fee schedule, not based on the actual cost to the clinician to acquire the drug. The methodology used by Medicare and most commercial payers to set the payment rates for individual drugs is known as ASP+x%: the clinician is paid the Average Sales Price for the drug two quarters earlier plus an additional percentage (6% extra in the Medicare program, typically more in commercial insurance contracts).
Back to top
C
CAH. See Critical Access Hospital
CAP. See Competitive Acquisition Program.
Capitation. A payment model in which a healthcare clinician is paid based on the number of individuals cared for, rather than on the number of services provided to those individuals. (The term capitation means that the payment is made “per person” or “per capita” rather than “per service.”) A capitation payment may or may not be “global.” In global capitation, the clinician is expected to deliver or arrange for all healthcare services the patient needs of any kind, but a capitation payment may also be defined to cover a specific menu of services or the services delivered by a subset of clinicians (the specific services that are covered are defined in a Division of Financial Responsibility). Alternatively, the capitation payment may be expected to cover all services except those of a specific type (i.e., some services are “carved out”). A capitation payment model needs to define a trigger (i.e., the circumstances that justify a particular clinician receiving the payment), the payments may differ for different patients (e.g., based on a risk adjustment system), and if multiple clinicians will be involved, a method of determining the accountable clinician is needed. In many traditional global capitation models, the trigger is the selection of a primary care physician, the group which employs that physician is the accountable clinician, and the payments are not risk adjusted, but different triggers can be used and the payments can be risk adjusted.
Condition-Specific Capitation. Condition-specific capitation is a form of capitation that is designed to cover only services provided for care of a particular health condition or combination of conditions. Condition-specific capitation is a form of Condition-Based Payment; in condition-specific capitation, a single payment or a single monthly payment is made for each patient who has the condition.
Contact Capitation. Contact capitation is a form of capitation that is triggered by a patient’s initial visit to a particular clinician and is intended to cover all services delivered by that clinician for a period of time or all services associated with the condition for which the patient is seeking care from the clinician. Contact capitation systems that were used in the 1990s paid a specific per-patient amount to a physician group for all of the services that physician group provided to a patient who came to the group seeking services for a particular health problem.
Global Capitation. Global capitation is a form of capitation in which the payment for each patient is intended to cover all services the patient needs for all of their health problems.
Partial Capitation. Partial capitation is a form of capitation in which some services, but not all, are to be delivered in return for a capitation payment, and other services are to be paid for separately. For example, professional services capitation is a form of partial capitation – a physician group or Independent Practice Association accepts a capitation payment to cover all professional services delivered by its physicians, including physician services delivered in hospitals, but the hospitals are still paid separately for their portion of hospital stays. The Affordable Care Act authorized the use of partial capitation payments to Accountable Care Organizations, but this portion of the law has not been implemented by CMS.
Percent of Premium Capitation. Percent of premium capitation is a capitation payment made by a health insurance plan to a clinician based on a pre-defined percentage of the insurance premiums collected for the health plan members assigned to the clinician. Under percent-of-premium capitation, the clinician is not only at risk for what kinds of health problems the patient has and how efficiently the clinician treats those problems, but it is also at risk for how well the premiums set by the health plan match the costs of treating the health problems of the members the health plan insures.
Primary Care Capitation. In a primary care capitation payment model, a per patient payment is made to a primary care practice to cover all services delivered by the primary care practice, but not to cover any services delivered by other clinicians. Under most primary care capitation systems, the primary care practice receives a monthly payment for each patient enrolled with the practice and does not bill separately for individual office visits with those patients.
Professional Services Capitation. Professional services capitation is a form of capitation in which the payment for each patient only covers professional services delivered by physicians or other clinicians, not services delivered by hospitals or other institutional clinicians. Professional services capitation is one type of partial capitation.
Risk-Adjusted Capitation. Risk-adjusted capitation is a form of capitation in which the amount of payment made for a particular individual differs depending on a measure of the types, volume, or cost that individual is expected to need. See Risk Adjustment for additional information.
Capitation vs. Global Payment. A capitation payment need not be “global;” for example, if a patient needs surgery, a Professional Services Capitation payment would only cover the payments to the surgeon, the anesthesiologist, and other physicians involved with the surgery, but not the payment to the hospital where the surgery was performed. Conversely, a global payment need not be paid using a “capitation” methodology; for example, a hospital might receive a global payment in the form of an annual budget payment that is expected to cover all of the services it delivers, regardless of how many individuals are in the community served by the hospital or how many services the hospital delivers to those community residents.
Carve-Out. A carve-out is a set of services that is paid for in a way that differs from the way payment is made for other services. For example, a single global payment might be paid to a clinician for all services, except for a list of specific services or conditions that would still be paid on a traditional fee-for-service basis or through individual bundled payments. A carveout may apply to the delivery of services as well as to payment. For example, many purchasers and payers have “carved out” behavioral health services and require that patients receive them from a different set of clinicians than the clinicians who deliver physical health services to the patients; the behavioral health clinicians are paid separately and in different ways than the clinicians who deliver physical health services.
Case Mix. Case mix is a general term used to describe the types of patients cared for by a clinician during a period of time. A case mix index is often calculated to assess whether a particular clinician is caring for patients who have more complex needs or who need more expensive services.
Case-Mix Groups (CMGs). Case Mix Groups (CMGs) is a risk adjustment system used in the Medicare payment system for Inpatient Rehabilitation Facilities (the Inpatient Rehabilitation Facility Prospective Payment System). There are 92 different CMG categories, and the patient is assigned to a category based on the diagnosis that led to their need for rehabilitation, their comorbidities, their age, and their functional and cognitive status.
Case Mix Index. The Case-Mix Index for a hospital measures the relative severity of the needs of its patients. The Case Mix Index is calculated by determining the DRG weight for each patient discharged from the hospital, adding all of those weights together, and dividing the sum by the total number of discharges.
Case Rate. A case rate is a generic term describing a single payment for all or most of the services a clinician delivers for a particular patient “case.” Although there is no one way to define a “case,” the term connotes care associated with a particular condition or procedure. For example, a single payment for a hospital stay (such as the DRG payments made in the Medicare Inpatient Prospective Payment System) and a global surgical fee are typically described as case rates.
CC. CC is an abbreviation for Complications and Comorbidities. See Diagnosis Related Groups.
CCO. See Coordinated Care Organization.
Center for Medicare and Medicaid Innovation (CMMI). The Center for Medicare and Medicaid Innovation (CMMI) was created by the Affordable Care Act to test payment models “where there is evidence that the model addresses a defined population for which there are deficits in care leading to poor clinical outcomes or potentially avoidable expenditures,” with a focus on “models expected to reduce program costs while preserving or enhancing the quality of care received by individuals.” The law also permits the Secretary to implement a payment model more broadly, including nationally, if the Secretary determines the payment model is expected to “reduce spending without reducing the quality of care or improve the quality of patient care without increasing spending” and if the Chief Actuary of CMS certifies that the expansion would reduce or not result in any increase in net federal spending.
The law contains the following list of 24 “innovative payment and service delivery” models that CMMI is specifically authorized to test on a demonstration basis, although CMMI is not limited to testing these models nor is it explicitly required to test any of them.
- Promoting broad payment and practice reform in primary care, including patient-centered medical home models for high-need applicable individuals, medical homes that address women’s unique healthcare needs, and models that transition primary care practices away from fee-for-service based reimbursement and toward comprehensive payment or salary-based payment.
- Contracting directly with groups of clinicians of services and suppliers to promote innovative care delivery models, such as through risk-based comprehensive payment or salary-based payment.
- Utilizing geriatric assessments and comprehensive care plans to coordinate the care (including through interdisciplinary teams) of applicable individuals with multiple chronic conditions and at least one of the following: (1) an inability to perform 2 or more activities of daily living; or (2) cognitive impairment, including dementia.
- Promote care coordination between clinicians of services and suppliers that transition healthcare clinicians away from fee-for-service based reimbursement and toward salary-based payment.
- Supporting care coordination for chronically ill individuals at high risk of hospitalization through a health information technology-enabled clinician network that includes care coordinators, a chronic disease registry, and home tele-health technology.
- Varying payment to physicians who order advanced diagnostic imaging services according to the physician’s adherence to appropriateness criteria for the ordering of such services, as determined in consultation with physician specialty groups and other relevant stakeholders.
- Utilizing medication therapy management services, such as those described in section 935 of the Public Health Service Act.
- Establishing community-based health teams to support small-practice medical homes by assisting the primary care practitioner in chronic care management, including patient self-management activities.
- Assisting applicable individuals in making informed healthcare choices by paying clinicians of services and suppliers for using patient decision support tools, including tools that meet the standards developed and identified under section 936 (c)(2)(A) of the Public Health Service Act, that improve applicable individual and caregiver understanding of medical treatment options.
- Allowing States to test and evaluate fully integrating care for dual eligible individuals in the State, including the management and oversight of all funds under the applicable titles with respect to such individuals.
- Allowing States to test and evaluate systems of all-payer payment reform for the medical care of residents of the State, including dual eligible individuals.
- Aligning nationally recognized, evidence-based guidelines of cancer care with Medicare payment incentives in the areas of treatment planning and follow-up care planning for individuals with cancer, including the identification of gaps in applicable quality measures.
- Improving post-acute care through continuing care hospitals that offer inpatient rehabilitation, long-term care hospitals, and home health or skilled nursing care during an inpatient stay and the 30 days immediately following discharge.
- Funding home health clinicians who offer chronic care management services to applicable individuals in cooperation with interdisciplinary teams.
- Promoting improved quality and reduced cost by developing a collaborative of high-quality, low-cost healthcare institutions that is responsible for (1) developing, documenting, and disseminating best practices and proven care methods; (2) implementing such best practices and proven care methods within such institutions to demonstrate further improvements in quality and efficiency; and (3) providing assistance to other healthcare institutions on how best to employ such best practices and proven care methods to improve healthcare quality and lower costs.
- Facilitate inpatient care, including intensive care, of hospitalized applicable individuals at their local hospital through the use of electronic monitoring by specialists, including intensivists and critical care specialists, based at integrated health systems.
- Promoting greater efficiencies and timely access to outpatient services (such as outpatient physical therapy services) through models that do not require a physician or other health professional to refer the service or be involved in establishing the plan of care for the service, when such service is furnished by a health professional who has the authority to furnish the service under existing State law.
- Establishing comprehensive payments to Healthcare Innovation Zones, consisting of groups of clinicians that include a teaching hospital, physicians, and other clinical entities, that, through their structure, operations, and joint activity deliver a full spectrum of integrated and comprehensive healthcare services to individuals while also incorporating innovative methods for the clinical training of future healthcare professionals.
- Utilizing, in particular in entities located in medically underserved areas and facilities of the Indian Health Service (whether operated by such Service or by an Indian tribe or tribal organization), telehealth services (1) in treating behavioral health issues (such as post-traumatic stress disorder) and stroke; and (2) to improve the capacity of nonmedical clinicians and non-specialized medical clinicians to provide health services for patients with chronic complex conditions.
- Utilizing a diverse network of clinicians of services and suppliers to improve care coordination for individuals with 2 or more chronic conditions and a history of prior-year hospitalization through interventions developed under the Medicare Coordinated Care Demonstration Project.
- Focusing primarily on physicians’ services furnished by physicians who are not primary care practitioners.
- Focusing on practices of 15 or fewer professionals.
- Focusing on risk-based models for small physician practices which may involve two-sided risk and prospective patient assignment, and which examine risk-adjusted decreases in mortality rates, hospital readmissions rates, and other relevant and appropriate clinical measures.
- Focusing primarily on Medicaid, working in conjunction with the Center for Medicaid and CHIP Services.
Centers for Medicare and Medicaid Services (CMS). The Centers for Medicare and Medicaid Services is the federal agency responsible for administering the Medicare and Medicaid programs and carrying out other functions with respect to healthcare and health insurance.
Center of Excellence. The term Center of Excellence is generally used to describe a particular service line of a specific clinician that has been determined in some way to provide higher quality services at the same or lower cost than other clinicians.
Center of Excellence Contract. In a Center of Excellence contract, a purchaser or payer contracts with a clinician that has been designated as a Center of Excellence to provide a specific set of services to the purchaser or payer’s members under a payment model for the clinician and a benefit design for the patient that differ from those used for other clinicians. For example, an individual member of the purchaser or payer who obtains a service from a Center of Excellence may have lower cost-sharing or no cost-sharing at all for using the service and may receive reimbursement for costs involved in traveling to and from the Center of Excellence.
CG-CAHPS (Clinician and Group Survey – Consumer Assessment of Healthcare Clinicians and Services). CG-CAHPS is one of a family of CAHPS surveys that ask consumers and patients to rate their experiences receiving care in a variety of healthcare settings. The CG-CAHPS survey is specifically designed for services delivered in physician offices. A growing number of payers are using results of CAHPS surveys as a performance measure in payment models. See also H-CAHPS.
Charge. The charge for a service is the payment amount that a clinician states that it wishes to receive in return for delivery of the service. In general, third-party payers require or negotiate with a clinician to accept a payment for a service that is lower than the charge. The actual payment is known as the allowed amount, and the difference between the allowed amount and the charge is the clinician’s discount. Self-pay patients may be required to pay the full charge unless they can negotiate a discount with the clinician.
Chargemaster. A list of the charges for all services in a hospital is known as a Chargemaster.
Cherry-Picking. Cherry-picking is a colloquial term used to describe a situation in which a healthcare clinician or payer seeks out patients for whom the cost of services is expected to be less than the payment for those services or the premium received for their health insurance. See also Lemon-Dropping.
Civil Monetary Penalty. The federal Civil Monetary Penalty statute imposes financial penalties on hospitals that make payments to physicians as an inducement to reduce or limit services to Medicare or Medicaid beneficiaries. The law has been interpreted by the Office of Inspector General (OIG) as prohibiting such payments even if the services being reduced are not medically necessary or appropriate. Consequently, gain-sharing programs designed to reward physicians for reducing unnecessary services or unnecessary elements of services could make a hospital liable for civil money penalties. (Gainsharing arrangements may also be in violation of the federal Anti-Kickback statute and the Stark law.) Although the law applies only to Medicare or Medicaid beneficiaries, the OIG has viewed it as prohibiting such payments even for commercially insured patients, since the assumption is that incenting changes in practice for commercial patients would likely also result in changes in practice for Medicare or Medicaid patients, or that the amounts of payment incentives for changing practices, even though applied only to commercial payments, would be set at levels designed to incent the changes for all patients. For more information, see Fraud and Abuse Laws.
CIN. See Clinically Integrated Network.
Claim. An invoice submitted by a clinician to a payer seeking payment for services delivered to a patient. Claims from physicians are filed using a CMS-1500 form and claims from hospitals are filed using a CMS-1450/UB-04 claims form.
Claims Data. Information that is recorded on the forms used to submit claims for payment. Two key types of information recorded on claims forms are (1) one or more procedure codes describing specific services the patient received, and (2) one or more diagnosis codes describing the problem that was being treated. The focus of the claims form is on the services delivered for payment, and so the diagnosis codes recorded on the claims form are not intended to be a comprehensive description of the patient’s health problems and other characteristics, but to describe the reasons for delivering the service for which payment is being sought.
Claims Runout. If information is being collected from claims data about services that were delivered during a specific period of time, the claims runout is an additional period of time that is allowed after the end of the period in which services are being measured in order to allow claims for those services to be filed. For example, if the claims runout is 90 days, then a measure of how many services were delivered or how much was spent on services during a calendar year is not calculated until at least 90 days after the end of the year. A longer claims runout provides more complete and accurate information about the measurement period, while a shorter claims runout provides information more quickly. (For more information, see Completion Factor and IBNR.) The term claims runout (or claims runoff) is also used to define the deadline or maximum period of time in which a claim must be submitted after a service is rendered in order to receive payment from a payer.
Clean Period. A “clean period” is a term used to define a specific length of time in which an individual receives no healthcare services related to a particular condition or treatment. If an episode of care is defined as all services related to a particular condition or procedure regardless of when the services were delivered, an episode grouper needs to have a way of determining when the episode has ended, so the episode grouper may be programmed to look for a clean period in order to make a determination that the episode has ended. Any service that occurs after the clean period is then assumed to be part of a new or different episode.
Clinical Data. Clinical data is information that is recorded about a patient and their care in a patient’s medical chart, in an electronic health record, or a clinical data registry. Two key types of information in clinical data are the types of services that a patient receives and the types of health problems a patient has. Clinical data generally have information about more services and more health problems than are available from claims data, since they will include services that are not eligible for individual payment and therefore are not described on claims forms, and they will also include information about health problems that were not explicitly treated by the clinician and may not be recorded on a claims form.
Clinically Integrated Network (CIN). A clinically integrated network is a term used to describe a collection of clinicians from different specialties who create processes and systems for managing and coordinating the care they deliver to individual patients. If a clinically integrated network meets specific standards established by the Federal Trade Commission (FTC), the clinicians in the network can jointly negotiate with payers in ways that could otherwise be deemed to be a violation of anti-trust laws, even if they are not taking financial risk. The things that a network must do to show it is clinically integrated under FTC rules include:
- Developing and using detailed, evidence-based clinical practice guidelines;
- Limiting participation in the network to clinicians who are committed to following the clinical practice guidelines;
- Measuring the participating clinicians’ compliance with the guidelines; and
- Enforcing use of the clinical guidelines.
Clinical Pathway. A Clinical Pathway (often called a “pathway” for short) is a set of appropriate use criteria and other clinical practice guidelines defining what types of services or procedures should be delivered to or ordered for specific patients. For example, a number of clinical pathways have been developed to guide decisions about the appropriate types of chemotherapy to use in treating cancer.
Clinical Pathway Program. A Clinical Pathway Program is a program designed to encourage clinicians to use a clinical pathway in choosing the services and procedures they deliver or order for patients. For example, in oncology, many payers require oncologists to use a clinical pathway in order for the oncologists to receive payment for treating cancer patients.
Clinical Practice Guidelines. Clinical practice guidelines are recommendations developed by a medical society or other organization to help physicians or other clinicians to deliver care efficiently and effectively. Guidelines will generally be based on evidence where it exists, but where evidence does not exist, guidelines may simply codify professional judgments about which treatments should be delivered. See also Appropriate Use Criteria and Clinical Pathway.
Clinical Resource Groups (CRG). Clinical Risk Groups (CRG) is a risk adjustment system developed by 3M Health Information Systems that uses a patient’s diagnoses and past medical interventions to determine whether the patient has chronic conditions or acute conditions or both and the severity of those conditions. This information is then used to assign the patient to one of 269 different “Base CRGs” and to one of up to 6 different severity levels, for a total of 1,080 potential different groupings.
CMG. See Case-Mix Groups.
CMMI. See Center for Medicare and Medicaid Innovation.
CMS. See Centers for Medicare and Medicaid Services.
CMS-1450. The CMS-1450 is the claims form used by hospitals to submit claims to Medicare for payment of healthcare services. The same form is known as a UB-04 for claims submitted to commercial payers.
CMS-1500. The CMS-1500 is the claims form used by physicians and other non-institutional clinicians to submit claims to payers for payment of healthcare services. (Hospitals submit claims using the UB-04 claims form.)
Co-Insurance. Co-insurance is a form of cost-sharing; the co-insurance amount is calculated as a percentage of the total allowed amount for a service. The patient is required to pay the co-insurance amount to a clinician in order to receive a service; the remainder of the payment to the clinician is then paid by the insurance plan or other payer. The patient is expected to pay an additional co-insurance amount each time an additional service is rendered (if the service requires co-insurance).
Comorbidity. A comorbidity is a health condition other than the condition being treated that may affect the cost of the treatment or the outcomes that can be achieved.
Competitive Acquisition Program. The Competitive Acquisition Program was a program created by Congress that was intended to control the cost of drugs administered in physician offices. CMS implemented the program in 2006 but suspended the program at the end of 2008 due to lack of participation by vendors and other problems.
Composite Measure. A composite measure is a measure of quality, utilization, or spending that is calculated based on performance on two or more other measures. There are two basic approaches to constructing composite measures:
All or Nothing Composite. In an all-or-nothing composite, if the performance threshold is not reached for a patient on one of the measures in the composite, then the clinician is deemed not to have achieved adequate performance for that patient on the composite measure. For example, in a composite measure of diabetes care called the D5 that is based on five separate individual measures, a 30% score for a clinician means that adequate performance was achieved on all five of the measures for 30% of the patients, and for 70% of the patients, adequate performance was not achieved on at least one of the 5 measures.
Weighted Average Composite. A weighted composite measure is constructed by multiplying each individual measure by a measure weight and then summing the products to create a composite measure score. A weighted average composite will generally have higher scores than an all-or-nothing composite, since the weighted average composite gives a clinician “partial credit” for a patient if adequate performance was achieved on some measures but not others. The relative rankings of clinicians on a weighted average composite will also depend on the measure weights if different clinicians have different levels of performance on different measures in the composite.
Comprehensive Care Payment. A Comprehensive Care Payment is a payment that is intended to support comprehensive services for a particular condition or group of conditions. A Comprehensive Care Payment is a form of Condition-Based Payment, but whereas a Condition-Based Payment could be designed to support a subset of the care needed for a condition, a Comprehensive Care Payment would support the full range of services the patient needs. For example, whereas a Condition-Based Payment for pregnancy might be limited to delivery of the baby (although it would not be based on the type of delivery in the way current physician and hospital payments are designed), a Comprehensive Care Payment would include prenatal care, delivery, and postpartum care services. (A global obstetrical fee covers that full range of services, but only includes the physician’s services, not the hospital’s services, whereas a Comprehensive Care Payment would include the services of all clinicians.)
Completion Factor. A completion factor is an adjustment made to a measure that was calculated based on claims data in order to compensate for claims that had not yet been filed by the time the measure was calculated. For example, if it is estimated that the claims for services that were delivered during the calendar year but submitted for payment more than 90 days after the end of the calendar year (i.e., services that are Incurred But Not Reported) represent 2% of the total amount that will ultimately be paid for all services delivered during the year, then the spending calculated based on the claims that were filed by 90 days after the end of the year (i.e., the Claims Runout period) would be increased by 2% to estimate what the spending would be once all claims were filed. See Claims Runout and IBNR.
Comprehensive Primary Care Initiative (CPCI). The Comprehensive Primary Care Initiative is a demonstration project implemented by the Center for Medicare and Medicaid Innovation in collaboration with private health plans in seven geographic regions to evaluate the impact of a specific change in the way primary care practices are paid. The primary care practices receive a per member per month (PMPM) payment in addition to current fee-for-service payments and can receive an additional shared savings payment if the total spending on all of the patients in all of the participating practices in their geographic region is lower than the spending in a comparison group of patients.
Concierge Medicine. Concierge medicine describes a mode of care delivery by a physician practice that provides more time with patients and more rapid response to requests for assistance than is possible under typical physician payment schedules, including longer office visits, phone calls, 24-hour access, etc. Typically, a patient pays a monthly, quarterly, or annual fee of some kind for concierge care in addition to fees for individual services, or the concierge fee may cover some services (such as office visits) but not other services.
Condition-Based Payment. Condition-based payment is a payment that is triggered by a patient’s health condition, rather than by delivery of a specific procedure or service delivered to address the condition. The “condition” may consist of more than one disease, particularly if the treatments for the diseases must be closely coordinated. For example, a condition-based payment could be paid for pregnancy care, rather than paying for a particular form of delivery; a condition-based payment could be paid for care of knee osteoarthritis, rather than for knee surgery, physical therapy, etc.; and a condition-based payment could be paid for management of heart failure and emphysema over a period of time.
Because patients with more severe conditions will likely need more services and because clinicians will have greater difficulty achieving good outcomes for them, condition-based payment models will generally need to incorporate some form of risk adjustment structure. (In a fee-for-service or treatment-based payment model, the services delivered serve as an implicit risk adjustment system, because a patient with greater needs will receive more services and that will generate higher payment. In a condition-based payment system, more direct measures of the patient’s needs must be used, such as the diagnoses assigned to the patient.)
Condition-Based Payment Code. A billing code that indicates that a physician or other clinician is managing the care of a health condition for a particular patient for a particular period of time and will serve as the Accountable Clinician for a Condition-Based Payment for that condition for that period of time.
Consumer Applications (Apps). Consumer apps include web-based and mobile software applications that help people manage their health and healthcare. Consumer apps refer to any electronic tool, technology, or system that:
- People select, use, and control without the input or involvement of their doctors, and outside of care delivery or management
- Interacts directly with people who provide personal health information to, and receive personal health information from, the tool, application, or system
- Allows the data, information, or recommendations to be used with, but is not dependent upon, a healthcare professional
Contact Capitation. See Capitation.
Conversion Factor. A conversion factor is a dollar amount that is multiplied by a relative value unit (RVU) or payment weight assigned to a particular service or bundle in order to determine the amount that will be paid to a clinician for delivering that service or bundle. For example, in the Medicare Physician Fee Schedule, two different services will be assigned two different RVUs, and those RVUs will be multiplied by the same conversion factor to determine the actual dollar amounts that Medicare will pay for those services. In the Medicare Inpatient Prospective Payment System, the payment for a hospitalization is determined by multiplying the weight for the DRG assigned to the patient by a conversion factor determined through a formula. The use of a Conversion Factor allows an entire set of payments to be uniformly updated for inflation while leaving the relative values among the services unchanged.
Contribution Margin. The contribution margin from a service is the difference between the payment received for delivery of the service and the variable cost to the clinician of delivering that service. The total contribution margin from all services is used to cover the clinician’s fixed costs, and then any funds remaining represent the clinician’s margin.
Coordinated Care Organization (CCO). A Coordinated Care Organization is a regional entity in the State of Oregon that includes both payers and clinicians and takes responsibility for managing the quality and cost of care for Medicaid patients living within the CCO’s defined region.
Co-Payment. A co-payment is a form of cost-sharing. It is a fixed dollar amount that a patient is required to pay to a clinician in order to receive a particular service; the remainder of the payment to the clinician is then paid by the insurance plan or other payer. The patient is expected to pay an additional co-payment each time an additional service is rendered (if the service requires a co-payment).
Cost. In terms of healthcare services and payment, the term “cost” is used to mean two very different things depending on the context in which it is used:
- The cost of a healthcare service to a patient, payer, or purchaser is the amount that individual or entity pays a clinician in return for the service being delivered. It is less confusing if this is referred to as a payer’s spending, because the payer may also incur other costs that are not directly associated with healthcare services, such as administrative costs.
- The cost of a healthcare service to a clinician is the amount that clinician pays to its employees, suppliers, etc. in order to deliver the service. Although this involves spending by the clinician for services delivered by others, it is less confusing if this is referred to as the clinician’s cost of delivering services.
It is desirable to use different terms for these two concepts – spending for the first and cost for the second– because the payer’s spending may be either higher or lower than the clinician’s cost. A clinician may be paid more than it costs to deliver a service, in which case the clinician also generates a profit margin. A payer may pay less than it costs clinicians to deliver a service, in which case the clinicians lose money.
Fixed Cost. The fixed cost of delivering a service is the component of costs incurred by a clinician that does not vary in proportion to the number of services delivered. For example, a hospital must spend money to furnish, equip, and maintain a surgery suite in order to do any surgeries at all; these costs will not change if one more or one fewer surgery is performed. Fixed costs are only “fixed” in the short run, however.
Semi-Variable Cost. The semi-variable cost of delivering a service includes aspects of cost that increase or decrease only if there are sufficiently large changes in the number of services delivered. For example, on a hospital nursing unit, an increase or decrease of one patient will generally not result in a change in the number of nurses needed to staff the unit, but if there is a large enough decrease in the number of patients, the hospital many need fewer nurses to safely staff the unit.
Variable Cost. The variable cost of delivering a service includes the aspects of costs incurred by a clinician that vary in proportion to the number of services delivered. For example, a hospital must purchase a knee implant device for each surgery to replace a patient’s knee, but it does not need to purchase an implant if no surgery is performed, so the implant is a variable cost. If one fewer surgery is performed, the hospital’s costs will decrease because it will need to acquire one fewer knee implant, and if more surgeries are performed, the hospital will need to spend more on knee implants.
Cost-Based Reimbursement. In a cost-based reimbursement system, a clinician calculates the total amount it spent to deliver one or more healthcare services for a patient, and the payer reimburses the clinician for those costs. If costs cannot be specifically associated with an individual patient, the clinician would calculate the total costs for delivering those services to all patients and then the payer would pay a percentage of those costs based on the percentage of the clinician’s total patients who are insured by that payer. For example, Medicare payments to Critical Access Hospitals are calculated as 101% of the portion of the hospital’s costs attributable to Medicare beneficiaries who received services from the hospital.
Cost-Sharing. Cost-sharing is the amount that a patient pays out-of-pocket to a healthcare clinician in return for a service, with no reimbursement from a third-party payer. The four principal approaches to cost-sharing are co-payments, co-insurance, deductibles, and balance billing.
Cost-Shift. “Cost-shift” is generally used to denote situations in which a particular payer pays less for a service than it actually costs a clinician to deliver that service, but rather than incurring a loss or not delivering the service at all, the clinician charges another payer more than the service actually costs (or charges more for a different service than that service costs) in order to offset losses from the payments made by the first payer. In effect, the clinician has “shifted” the costs associated with services for the first payer to the second payer or from the one service line to the other service line.
Cost-to-Charge Ratio. The cost-to-charge ratio is calculated by dividing a clinician’s reported total expenses during a period of time by the sum of the charges associated with all of the services delivered during that period of time. The cost-to-charge ratio is often used to estimate the cost of a specific service from the clinician’s charge for that service by multiplying the charge by the cost-to-charge ratio. However, in general, the amount a clinician charges for a particular service bears no systematic relationship to the cost of delivering that service (moreover, the cost of delivering the service will depend on the volume of services delivered), so service-specific costs estimated in this way are likely inaccurate.
Covered Service. A covered service is a healthcare service that a patient’s health insurance plan will pay a healthcare clinician to deliver.
CPCI. See Comprehensive Primary Care Initiative.
CPR. See Customary, Prevailing, and Reasonable.
CPT®. See Current Procedural Terminology.
CPT Editorial Panel. The CPT Editorial Panel is a committee appointed and staffed by the American Medical Association to oversee the addition, deletion, and modification of CPT Codes.
CRG. See Clinical Resource Groups.
Critical Access Hospital. A Critical Access Hospital is a hospital with fewer than 25 acute inpatient beds located in a rural area and distant from other hospitals. In contrast to larger hospitals that are paid through the Medicare Inpatient Prospective Payment System, Critical Access Hospitals are paid using a cost-based reimbursement model.
Current Procedural Terminology (CPT®). Current Procedural Terminology is a listing of definitions and alphanumeric codes for reporting medical services and procedures performed by physicians. It is maintained by the American Medical Association under the supervision of the CPT Editorial Panel. The CPT system was first developed in 1966; in 2000, it was designated by the U.S. Department of Health and Human Services as the national coding standard for services and procedures delivered by physicians and other healthcare professionals.
CPT® Category I. CPT® Category I consists of the principal codes used to document services that are delivered by physicians and that are used to bill for payment for those services. Examples of CPT Category I Codes are:
- 99203: Office or other outpatient visit for the evaluation of a new patient which involves a detailed history, a detailed examination, and medical decision making of low complexity.
- 27590: Amputation of the leg through the femur.
CPT® Category II. CPT® Category II codes are codes used for performance measurement. They facilitate documentation that a particular task was performed (e.g., that the patient’s blood pressure was measured) as part of an evaluation and management service that is billable using a CPT Category I code, or documentation of a patient condition, test result, or treatment outcome (e.g., whether the patient’s blood pressure was high or low). A CPT Category II code is not intended to be used as a billing code for payment, but a payment model may be structured to modify the payment amount for a service described by a CPT Category I code based on whether a CPT Category II code indicates that a task was performed as part of that service, an outcome was achieved as a result of that service, or a particular patient condition was present. Examples of CPT Category II codes are:
- 2000F: Blood pressure measured
- 3074F: Most recent systolic blood pressure less than 130mm Hg
CPT® Category III. CPT® Category III codes are temporary codes for emerging technology, services, and procedures. They are designed to allow data collection for these services in a systematic way. Examples of CPT Category III codes are:
- 0071T: Focused ultrasound ablation of uterine leiomyomata, including MR guidance; total leiomyomata volume less than 200 cc of tissue.
- 0223T: Acoustic cardiography, including automated analysis of combined acoustic and electrical intervals; single, with interpretation and report.
Customary, Prevailing, and Reasonable (CPR). Prior to the creation of the Resource Based Relative Value Scale (RBRVS), Medicare payments to physicians were based on Customary, Prevailing, and Reasonable (CPR) charges. The CPR system was based on the UCR (usual, customary, and reasonable) concept, but it included specific metrics for determining “customary,” “prevailing,” and “reasonable.” (“Customary” was defined as the median of an individual physician’s charges for a service over a particular period of time; “prevailing” was defined as the 90th percentile of the customary charges for all physicians in the same specialty in a geographic area, and “reasonable” was defined as the lowest of the actual fee, the customary charge, and the prevailing charge.)
Back to top
D
Deductible. A deductible is a form of cost-sharing. Under a health plan with a deductible, the patient is required to pay 100% of the cost of all services until the patient’s total spending reaches the deductible, at which point other cost-sharing rules such as copayments and co-insurance apply. Some services, such as preventive care services, may be exempt from the deductible requirement, and for those services the patient may be expected to pay other forms of cost-sharing, or the patient may have no cost-sharing at all.
Delivery System Reform Incentive Payment (DSRIP) Program. A Delivery System Reform Incentive Payment Program is a special pool of funds that can be used by a state Medicaid program to encourage or support changes in care delivery by hospitals and other clinicians to Medicaid beneficiaries and other low-income individuals. The programs are created on a state by state basis through Section 1115 Medicaid waivers approved by the Centers for Medicare and Medicaid Services.
Denominator Exclusion. In a performance measure, if the measure focuses on a particular subset of patients, or if there is a reason why performance should not be measured for a particular patient or a patient with particular characteristics, patients who should not be measured are excluded from both the numerator and denominator of the measure. For example, if one is calculating the percentage of diabetic patients who have had their blood pressure measured, then non-diabetic patients are excluded from the denominator as well as the numerator.
Designated State Health Program (DSHP). A program approved in some states under Section 1115 Waivers to allow Federal Medicaid funding to be used for services that are not typically eligible for such funding.
Diagnosis Related Groups (DRGs). Diagnosis Related Groups (DRGs) is a system of classifying patients into categories based on their expected relative use of inpatient hospital services. A version of DRGs called MS-DRGs is used as part of the Medicare Inpatient Prospective Payment System (IPPS) to pay hospitals for inpatient admissions of Medicare beneficiaries, and a version called APR-DRGs is used by many commercial health insurance plans to pay hospitals for admissions of their members. DRGs are a clinical category risk adjustment system that uses information about patient diagnoses and selected procedures to identify patients that are expected to have similar costs during a hospital stay. Each DRG is assigned a weight that reflects the relative cost of caring for patients in that category relative to other categories. The weight assigned to a DRG may differ for different payers if they have different patient populations, since weights are typically determined by calculating the average costs for caring for patients in each category relative to all patients in a population of patients.
In current versions of DRGs, there may be two or three different DRGs defined for any major condition or procedure, based on whether the patient has other health problems (called comorbidities) that would affect services and spending for treatment of that specific condition or delivery of that specific procedure, or if the patient experiences complications during the hospital stay. If there are three DRGs for patients with a specific condition or surgical procedure, one of the DRGs is for patients without complications or comorbidities (abbreviated as “w/o CC/MCC”), a second DRG is for patients with complications or comorbidities that are not classified as major (abbreviated as “w CC”) and a third DRG is for patients with major complications or comorbidities (abbreviated as “w MCC”). If there are only two DRGs for a condition or procedure, one is used for patients without major complications (abbreviated as “w/o MCC”) and one is for patients with major complications (abbreviated as “w MCC”).
DRGs can be used as a risk adjustment system for both payment and performance measurement; for example, DRGs are used to calculate an overall risk score for a hospital called a Case Mix Index, which is the sum of the DRG weights for all patients discharged from the hospital divided by the total number of discharges. DRGs are also used as bundled payments/ case rates; in the Medicare IPPS and other payment models, the hospital receives a single “DRG payment” for a patient admitted to the hospital that is intended to cover all of the hospital’s costs of caring for that patient, with the payment amount for each patient determined by multiplying the DRG weight by a conversion factor.
Direct Contracting. Direct contracting is an arrangement between a purchaser and a clinician to deliver healthcare services for the purchaser’s members in return for payment specified in a contract with the purchaser rather than in a contract with a separate health insurance company. A direct contract may be focused on particular types of services, e.g., the purchaser may agree to pay a clinician for knee replacement surgeries performed on the purchaser’s members, or a direct contract may involve an agreement by the clinician to deliver or arrange for all or most types of health services for the purchaser’s members. In general, in order to have direct contracting for a broad range of services, the clinician will need to have a clinician-owned health plan that can manage the benefits and payments or the purchaser and clinician will need to jointly agree to use a third-party administrator to manage the terms of the contract.
Direct Primary Care. Direct Primary Care (DPC) is a term used to describe a payment model in which a primary care practice charges a monthly, quarterly, or annual fee to a patient that covers all or most of the services the primary care practice provides to the patient, including patient visits, laboratory testing, care management, etc., and there are no separate fees charged for individual services. Direct primary care is a bundled capitation payment, but with the payment coming from the patient rather than a health plan. In contrast, “concierge medicine” is typically a structure where a patient pays a fee of some kind in addition to fees for individual services, with the additional fee assuring that the patient will receive services that would not otherwise be possible under current fee schedules, including longer visits, phone calls, 24-hour access, etc.
Discounted Payment. A discounted payment is a payment to a clinician for a service from one payer that is lower than the amount other payers pay for the same service.
Dispensing Fee. A dispensing fee is a payment to a pharmacy from a pharmaceutical insurance plan or other payer for each medication that the pharmacy dispenses to a patient insured by the plan or paid for by the payer. The payment is intended to cover the costs of the pharmacy’s operations other than the cost of acquiring the drug itself. The dispensing fee is paid in addition to whatever mechanism is defined for paying the pharmacy for its cost of acquiring the drug.
Disproportionate Share Hospital. A hospital which has a higher-than-average number of Medicaid patients or a large number of low-income patients is classified as a “Disproportionate Share Hospital” and is eligible to receive additional payments.
Division of Financial Responsibility (DOFR). A division of financial responsibility (DOFR) is an agreement between a payer and a clinician, or between a payer and multiple clinicians, as to which services delivered by which clinicians are to be covered by a bundled payment or capitation model that covers some but not all services or clinicians. For example, the DOFR for a professional services capitation payment model would define which services are considered “professional services” that are covered by the capitation payment and which services would be paid separately. A DOFR will typically use service/procedure billing codes and diagnosis codes to define which services will be paid through the bundled payment and which will be paid in a different way.
Doughnut Hole. A “doughnut hole” is a feature of a benefit design in which a patient who has received services that exceed a certain threshold of spending is responsible for higher cost-sharing for subsequent services than the patient was responsible for paying prior to that point, but where the cost-sharing then declines again after a second threshold of spending is met. The Medicare Part D drug insurance program has had a “doughnut hole” that requires seniors to pay almost the full cost of drugs for a period of time after they have reached a certain spending level on drugs.
Downside Risk. See Risk.
DRG. See Diagnosis Related Group.
DRG Grouper. A DRG grouper is a computer program that takes all of the diagnosis codes and procedure codes assigned to a patient during a hospital stay and uses them to assign the patient to a particular Diagnosis Related Group (DRG) based on the official rules for making such assignments.
DRG Weight. A DRG weight is a value assigned to a specific Diagnosis Related Group (DRG) that indicates the relative amount of resources or spending that is expected to be used for patients classified in that DRG. An advantage of a clinical category system such as DRGs is that the same categories can be used for payments to different clinicians or different patient populations but with different weights based on their different costs. For example, Medicare uses the same MS-DRG categories for paying both acute care hospitals and long term care hospitals, but different weights are assigned to the same MS-DRG in each payment system because of the different costs of care in the two different types of facilities.
DSH. See Disproportionate Share Hospital.
DSRIP. See Delivery System Reform Incentive Payment.
Dual Eligible. An individual is said to be “dual-eligible” if he or she is eligible for both Medicare and Medicaid benefits. Although they are often discussed as though they were a homogeneous class of individuals, dual eligibles are very diverse because of the different ways that individuals can become eligible for both Medicare and Medicaid. For example, dual eligibles include young, disabled adults; poor, but relatively healthy older adults; and frail elderly living in nursing homes who have exhausted their incomes paying for long-term care services that are not covered by Medicare.
Back to top
E
E&M. See Evaluation and Management Services.
ECR®. See Evidence-Informed Case Rate.
Encounter. An encounter is an interaction between a clinician and a patient. In a capitation payment model or other payment model that does not tie payment to the specific number or types of services delivered, a payer may still wish to know what services were delivered, so instead of submitting a claim for each service (since a claim is generally associated with a payment), a clinician may be asked to submit a form documenting an encounter. Encounters include services that would be eligible for payment under a fee-for-service payment model, but they may also include other services or interactions that are not typically paid for under fee-for-service, such as telephone calls or e-mails with patients.
End-Stage Renal Disease Prospective Payment System (ESRD PPS). The End-Stage Renal Disease Prospective Payment System (ESRD PPS) is the payment system Medicare uses to pay outpatient dialysis centers for care of patients with end-stage renal disease (ESRD). Under the ESRD PPS, a separate payment is made for each dialysis treatment. The payment is a bundled payment that covers the costs of administering dialysis to a patient and the costs of ESRD-related drugs, laboratory services, and medical equipment and supplies. Oral-only ESRD-related drugs are excluded from the bundle but scheduled to be added in 2024. The payment covers two different methods of dialysis – hemodialysis and peritoneal dialysis – and covers dialysis whether it is administered in a dialysis center or in the patient’s home.
The amount of payment for a dialysis treatment is determined by adjusting a national base payment rate for geographic differences in costs using the Hospital Wage Index, then further adjusting for characteristics of the patient (age, body mass index, body surface area, and the presence of six specific comorbidities). The payment is also increased for treatments during the first four months of dialysis for a patient and for treatment at low-volume dialysis facilities. An additional outlier payment is paid if the cost of treating the patient exceeds an outlier threshold, and an additional payment is made for training patients to self-administer dialysis. The payments are reduced by up to 2% based on dialysis facilities’ achievement and improvement on specified quality measures.
The ESRD PPS is a single-clinician treatment-based bundled payment. It bundles together a series of services related to a single treatment. The bundle does not include the cost of physician services associated with the dialysis treatment. Although the number of services included in the bundle has increased over time, the bundled payment does not include any costs of complications of treatment and it does not cover an episode of care longer than the treatment itself. It includes a pay-for-performance penalty component based on quality.
Episode. The word “episode” is used in two somewhat different ways in the context of payment models:
- The care delivered during a fixed period of time. A common use of the word episode is to describe a period of time in which multiple services are delivered, all of which are related to a specific health problem or group of problems. The time period may be arbitrarily defined with no relation to the actual length of the patient’s treatment (e.g., a month, 60 days, or a year) and the episode may or may not include either the beginning or the end of a patient’s care for the condition or the delivery of the procedure involved.
- The complete set of related services for a condition or a procedure. The word episode is also used to describe all of the services that are needed to care for a particular condition or to complete the delivery of a procedure involving multiple services over a period of time. For example, if a patient receives surgery, the episode could include the surgery itself and any follow-up care that is related to the surgery or to complications of the surgery. To distinguish this from the other use of the word, this might be more clearly described as a “complete episode.”
An episode can be defined to be triggered by the presence of a particular patient condition (e.g., diabetes) or by the delivery of a particular service or procedure (e.g., heart surgery). A “complete episode” is ordinarily only defined in relation to an acute condition that appears at a particular point in time and is resolved at a later point in time. When the term episode has been used to describe the services related to a chronic condition that continues indefinitely, it has typically been defined as the services related to that condition that occur during a calendar year, even though other services related to the same condition were provided before and/or after the episode period. Limiting episodes to a year or less facilitates the use of payment contracts that are one year in length since many patients change health plans from year to year.
Episode (of Care) Payment. An “episode payment” or “episode of care payment” is a payment intended to cover all or most of the services delivered during an episode of care. The services covered by the episode payment will depend on how the episode of care is defined. For example, an Episode of Care Payment for knee surgery might be defined to include the services related to the surgery itself, the services delivered in the hospital for recovery from the surgery, the rehabilitation services the patient receives during and after discharge from the hospital to regain the ability to use the repaired knee, and services needed to address any infections or other complications that arise from the surgery. If the episode is not a “complete episode” but rather an arbitrary period of time, then the episode payment covers the services that occur during that period of time, and services that occur before or after that time period are paid with an additional episode payment or through some other means.
Episode Grouper. An episode grouper is an algorithm, typically implemented as part of a software system, that retrospectively examines individual claims for services and determines whether they fall within the definition of one or more episodes of care. Since claims forms are not designed to indicate the type of episode for which a service was delivered, episode groupers typically rely heavily on the diagnosis and procedure codes recorded on claims and on the relative timing of various services to determine which types of episodes have occurred and how to assign individual claims to those episodes; this can result in errors in determining which types of episodes have occurred and can cause services to be erroneously assigned to episodes.
Episode Length. The episode length is the number of days or months defined to be included in an episode of care. If a clinician is accepting an Episode (of Care) Payment, the episode length is the period of time in which services are expected to be covered by the episode payment rather than billed separately for individual payments. An episode length can be defined as a fixed or variable amount. In a fixed-length episode, the episode is the same fixed length of time for all patients, e.g., a year, and any related services that occur during that time period are included in the episode. A variant of this approach is to define an episode as a fixed length of time after completion of a particular service; for example, the episode length might be defined as 90 days after discharge from the hospital, in which case the actual length of the episode will depend on the length of time the patient spent in the hospital. In a variable length episode, the length of the episode varies from patient to patient. For example, if the episode is defined as ending when all related services have been delivered, then the length of the episode for a patient will depend on how long it took to deliver all of those services, whether the patient experienced complications that required additional services, etc. Variable length episodes are often terminated after a “clean period” occurs in which no related services are delivered. (See Clean Period.)
Episode Spending Measure. An episode spending measure calculates how much was spent on services for a patient during an episode of care. The clinicians who deliver the services to the patient may be paid under traditional fee-for-service payment models, and the episode spending measure may then be used to modify the amount of the fee-for-service payments to a clinician in some way based on whether the amount of spending in the episodes in which that clinician was involved is viewed to be high or low. For example, CMS is using several episode spending measures in its Hospital Value-Based Purchasing Program and Physician Value-Based Modifier Program to increase and decrease payments to hospitals and physicians based on the levels of spending in the episodes they were involved in relative to the levels of spending on similar episodes that other hospitals and physicians were involved in.
Some payers are using “episode spending measures” that include services that may be unrelated to the hospitalization or other service that triggered the episode. For example, the Medicare Spending Per Beneficiary measure includes the spending on all services received by a Medicare beneficiary during the 30 days following their discharge from the hospital, including services for conditions different from those that were treated during the hospital stay and services for conditions that may have first developed after the patient was discharged from the hospital.
ESRD PPS. See End Stage Renal Disease Prospective Payment System.
Evaluation and Management Services (E&M). The Current Procedural Terminology (CPT®) system defines codes for a range of different services that are collectively referred to as Evaluation and Management Services. The most commonly used Evaluation and Management (E&M) Services codes are for patient visits to a physician for evaluation of a symptom or management of a condition. If the physician carries out a specific test or performs a particular procedure during the visit, a separate procedure code would be billed for that service.
Evidence-Based Medicine. The term “evidence-based medicine” is used to describe the processes for determining which healthcare services a patient should receive based on explicit consideration of research showing whether a service is effective or which services are more effective. Contrary to popular belief, there is rarely evidence that “proves” a treatment will work or that a particular service is the best possible way to treat a patient; most evidence merely indicates that one treatment is more effective than others, on average, for a group of patients with particular characteristics. There are also different levels of evidence, with different levels of confidence as to the reliability of the results.
Evidence-Informed Case Rate (ECR). An Evidence-Informed Case Rate is a methodology developed by the Healthcare Incentives Improvement Institute (HCI3) for defining an appropriate amount of spending on a particular health condition. ECRs have been defined for both acute conditions and chronic conditions, and each ECR defines an episode of care that includes services related to the triggering condition delivered over a period of time. A key element of the ECR is the identification of services within the episode of care that are classified as Potentially Avoidable Complications (PACs), so that performance measures and payments can be defined separately for PAC services. ECRs incorporate a regression-based risk adjustment system for determining how the spending level should vary based on patient comorbidities.
ECRs are used as part of the PROMETHEUS payment model but they can also be used for measuring spending as part of a pay-for-performance system or other payment model. Many of the payments based on ECRs are a form of Condition-Based Payment, since many ECRs are triggered by a patient’s condition (as defined by diagnosis codes recorded on claims forms) rather than by the specific procedures delivered.
Exclusion (of Outliers). Exclusion is a statistical process that completely drops the most extreme values from a distribution. For example, in any group of patients with a particular condition, some patients may have unusual problems that require a large number of expensive services for that condition (“outlier patients”). If a clinician is given a fixed payment to pay for as many services as the patients need for the condition, the small number of patients requiring the large number of expensive services could cause losses for the clinician. This problem can be mitigated by not requiring the clinician to be responsible for the costs of the patients who are excluded. The threshold for exclusion can be set at a relative level (e.g., patients with costs above the 99th percentile) or at an absolute level (e.g., patients with costs above $100,000). See also Exclusion vs. Outlier Payment vs. Truncation vs. Winsorization.
Exclusion (of Services). In a global payment model, some specific services may still be paid separately and thereby are excluded from the global payment arrangement. See also Carve Out.
Exclusion vs. Outlier Payment vs. Truncation vs. Winsorization. If a clinician is given a fixed payment to pay for as many services as patients need, outlier patients (i.e., patients who need an unusually large number of services or unusually expensive services) can cause losses for the clinician. Exclusion of the outlier patient means the clinician is not expected to pay for any of the services to the outlier patient from the fixed payment. Truncation means that the clinician is only expected to pay up to a fixed amount for such patients (e.g., $100,000). Winsorization means that the clinician is only expected to pay up to the amount at a particular point in the distribution of spending for all patients (e.g., the 99th percentile). An outlier payment is an additional payment to the clinician to cover a portion of the costs of the services needed by the patient.
Back to top
F
Facility Fee. A facility fee is an additional charge for a healthcare service when it is delivered in a hospital or other facility that bills for its services separately from the physician or other clinician who actually performs the service.
Facility-Independent Payment. A facility-independent payment pays the same amount in the same way for a particular service or procedure regardless of the type of facility where the service or procedure is delivered, instead of separate payment systems or different payment amounts for the same service depending on whether it performed in a hospital or an ambulatory surgery center or physician office. A facility-independent payment may require a different risk adjustment system than facility-specific payments in order to distinguish patient characteristics that may require use of a more expensive setting for care.
Federally-Qualified Health Center Prospective Payment System (FQHC PPS). A Federally Qualified Health Center (FQHC) is an outpatient clinic that serves lowincome populations and meets specific federal requirements. Under the Federally-Qualified Health Center Prospective Payment System (FQHC PPS), Medicare pays an FQHC a bundled payment for each patient visit to the clinic instead of separate payments for individual services under the Physician Fee Schedule. Different types of visits are paid different amounts, and CMS has established a series of HCPCS G-Codes that FQHCs use to indicate what type of visit a patient received. For example, G0466 indicates that the visit was made by a new patient, G0467 indicates that the visit was made by an established patient, and G0469 indicates that the visit was for a new patient who received a qualified mental health service during the visit. Although the payments under the FQHC PPS are not tied directly to specific types of services, the patient must still make a visit to the clinic in order for the clinic to receive a payment.
Fee for Service Payment. A fee-for-service payment model is one in which a specific amount is paid when a particular service is delivered, and generally where the payment amount differs depending on which specific service is delivered.
Although fee-for-service payment systems are criticized for “rewarding volume over value,” many alternative payment models have similar characteristics. For example, most bundled payment and episode payment systems are triggered by the delivery of a service, so they still pay more if that service is delivered more frequently. Moreover, many of the services paid for under fee-for-service payment models are already bundled in some way (for more information, see Fee for Service Payment vs. Bundled Payment).
The problems with existing fee-for-service systems that need to be corrected by alternative payment models tend to fall in to two broad categories:
- Lack of payment or inadequate payment for high-value services. Despite the name, most fee-for-service payment system only pay fees for a subset of services that are of value to patients. For example, Medicare and most health plans don’t pay:
- for physicians to respond to a patient phone call about a symptom or problem, even though those phone calls can avoid far more expensive visits to the emergency room.
- for primary care physicians and specialists to coordinate care by telephone or email, even though lack of care coordination will result in the payers paying for duplicate tests and the problems caused by conflicting medications.
- for services delivered by nurses and other non-physician staff or for non-medical services that could help patients manage chronic conditions better and avoid expensive hospitalizations.
- Financial penalties for delivering a different mix of services. Under the fee for service system, clinicians lose revenue if they perform fewer procedures or lower-cost procedures, but their costs for delivering the remaining services generally do not decrease proportionately, and that can cause operating losses for the clinicians. Most fundamentally, under the fee for service system, clinicians don’t get paid at all when their patients stay healthy and don’t need healthcare services.
First Dollar Shared Savings. In a shared savings payment model, if the clinician’s share of savings is calculated based on the total amount of savings generated, it is said to receive “first dollar shared savings.” This is in contrast to a structure where the payer keeps all of the initial savings until a certain threshold is reached and only then shares additional savings with the clinician. However, even a first dollar shared savings model may not guarantee that a clinician will receive a share of savings no matter how the small the savings are. For example, in the Medicare Shared Savings Program, the savings must exceed the Minimum Savings Rate in order for an Accountable Care Organization to be eligible for any shared savings payment, but if the Minimum Savings Rate is achieved, then the share of savings is calculated based on the total savings achieved.
FMAP. FMAP is an abbreviation for Federal Medical Assistance Percentage, which is the percentage of a state’s Medicaid spending that the Federal government will pay for.
FQHC. FQHC is an abbreviation for Federally Qualified Health Center.
Fraud and Abuse Laws. The federal government and many state governments have enacted a series of laws designed to control fraud and abuse in healthcare payment. In some cases, the concerns about potential abuses under current payment systems may not exist (or may be significantly less) under a different payment model. However, because the fraud and abuse law is not tied to a particular payment model, the restrictions in the law can serve as a barrier to delivering care or distributing funds in different ways under the different payment model.
The principal federal fraud and abuse laws are:
- The Anti-Kickback statute;
- The Civil Monetary Penalty statute; and
- The Ethics in Patient Referrals Act, commonly known as the “Stark Law.”
The Affordable Care Act authorized CMS to grant waivers of these and other laws to clinicians participating in alternative payment models where necessary.
Formulary. In health insurance, a formulary is a list of pharmaceuticals that a health insurance plan will pay for. If a physician orders a medication that is not on the formulary, the physician will need approval from the payer to use the medication or the patient may have to pay the full cost of the medication.
For a hospital or other clinician, a formulary is a list of pharmaceuticals that will be maintained in inventory and used in patient care.
Fully-Insured. An employer or other purchaser is said to be fully-insured if they purchase a health insurance policy for each of their employees or members and pay premiums to a health insurance company to cover the costs of claims for healthcare services. For contrast, see Self-Insured.
Back to top
G
GAF. See Geographic Adjustment Factor.
Gain-Sharing. A gain-sharing payment is made by one clinician to another clinician if the first clinician experiences savings or higher profits due to actions taken by the second clinician. For example, if a physician redesigns care delivery in a way that reduces the costs the hospital incurs and thereby increases the hospital’s profit margin, the hospital could make a gain-sharing payment to the physician from those increased profits. A gain-sharing arrangement will generally require agreement between the two clinicians as to how costs and “gains” are to be measured. See also Fraud and Abuse Laws and Shared Savings vs. Gain-Sharing.
G-Code. A G-Code is a subset of the Level II codes that CMS creates and maintains as part of the Healthcare Common Procedure Coding System (HCPCS). G-codes define procedures and professional services that Medicare will pay for but that have not been incorporated into the CPT coding system. Examples of GCodes are:
- G0008: Administration of influenza virus vaccine.
- G0257: Unscheduled or emergency dialysis treatment for an ESRD patient in a hospital outpatient department that is not certified as an ESRD facility.
Geographic Adjustment Factor (GAF). A Geographic Adjustment Factor is a number that indicates how much more will be paid for a service in one geographic area compared to other geographic areas based on differences in the cost of living and cost of purchasing services needed in the delivery of medical care. In the Medicare Program, payments to hospitals and other clinicians are adjusted by the Hospital Wage Index, and physician payments are adjusted using three separate factors used called Geographic Practice Cost Indices (GPCIs).
Geographic Practice Cost Index (GPCI). In the Medicare Physician Fee Schedule, in order to determine the actual dollar payment to an individual physician for a service, the Work, PE, and PLI RVUs are each adjusted by a corresponding Geographic Practice Cost Index that is intended to reflect differences in the costs of living, operating a practice, and obtaining insurance in different geographic areas of the country.
Global Budget. A global budget is an amount of money that is expected to cover all or most of the services that a patient needs from all clinicians during a particular period of time. In a global budget payment model, clinicians continue to bill for and be paid through the payment models that are typically used for the services. After the end of the time period for which the global budget is defined, all of the payments made to all clinicians for services covered by the global budget are tabulated and compared to the global budget in a retrospective reconciliation process. If the total payments are below the global budget, the payer pays the difference to the clinician or organization that has accepted accountability for the budget, and if the total payments exceed the budget, then the accountable clinician is responsible for reimbursing the payer for the overage.
Global Fee. A global fee is a single payment made to one clinician for performing a group of services over a period of time (the global period) instead of paying the clinician individual fees for the individual services. For example, surgeons receive a global surgical fee which covers a visit with a patient before the surgery is performed and visits with the patient after the surgery is completed, and a surgeon receiving the global fee does not bill for separate fees for the individual visits. Similarly, obstetricians receive a global fee that covers prenatal care, delivery, and postpartum care, and the obstetrician receiving the fee does not bill separately for the individual prenatal and post-partum care visits.
Global Budget vs. Shared Savings. A key difference between a Global Budget and a typical Shared Savings program is that the Global Budget is defined prospectively while the target spending level needed to receive shared savings is defined retrospectively. Under a Global Budget, the accountable clinician knows in advance what level of spending will be within the Global Budget and can monitor spending and take actions to help keep spending under that level. In contrast, under a Shared Savings Program, the clinician does not know in advance what the target spending level is; “savings” are declared to have been achieved if spending on the accountable clinician’s patients has decreased more or increased less than spending has changed for other clinicians’ patients, but the latter is only known after the fact.
Global Payment. A global payment is a payment that covers all or most of the services that a patient needs from all clinicians during a particular period of time. The term “global payment” is generally used in reference to a payment that covers multiple episodes of care for multiple types of conditions, whereas the term “episode payment” is used for a payment that is limited to a particular time period or to care associated with a particular procedure, and the term “condition-based payment” is used for a payment that is limited to a specific patient health condition or group of conditions.
Risk-Adjusted Global Payment. In a risk-adjusted global payment model, the amount of global payment a clinician receives is adjusted up or down based on the risk or acuity level of the individuals whose care is to be covered by the global payment.
Global Payment vs. Global Budget. In many cases, particularly when independent clinicians are involved with a “global payment,” the payment will actually be implemented using a global budget process, since this avoids the need for the clinician who is accountable for the global payment to pay claims from other clinicians that deliver services that are to be covered by the global payment. If the accountable clinician has a clinician-owned health plan, then it is in a better position to accept a global payment and directly pay claims from other clinicians.
Global Payment vs. Global Fee. A global payment usually refers to a payment that supports services delivered by multiple clinicians, whereas a “global fee” usually refers to a bundle of services delivered by one clinician.
Global Period. A Global Period is a period of time in which services delivered by a clinician are covered by a Global Fee rather than separately billed for individual service fees.
GPCI. See Geographic Practice Cost Index.
Back to top
H
HAC. See Hospital-Acquired Condition.
HCAHPS (Hospital Survey – Consumer Assessment of Healthcare Clinicians and Services). HCAHPS is one of a family of CAHPS surveys that ask consumers and patients to rate their experiences receiving care in a variety of healthcare settings. The HCAHPS survey is specifically designed for services delivered in hospitals. A growing number of payers are using results of CAHPS surveys as a performance measure in payment models. See also CG-CAHPS.
HCPCS. See Healthcare Common Procedure Coding System.
Healthcare Common Procedure Coding System (HCPCS). The Healthcare Common Procedure Coding System is a comprehensive set of billing codes maintained by the Centers for Medicare and Medicaid Services in accordance with the Health Insurance Portability and Accountability Act of 1996 (HIPAA). HCPCS Level I codes are the Current Procedural Terminology (CPT) codes developed and maintained by the American Medical Association, and HCPCS Level II codes are additional billing codes for additional services and medications not covered by the CPT system.
Herfindahl-Hirschman Index. The Herfindahl-Hirschman Index is a measure of the concentration of buyers or sellers in a geographic area. It is often used by economists and anti-trust enforcement agencies to assess whether a consolidation of clinicians or payers in a state or region, or an organizational arrangement to allow joint contracting with a group of clinicians (such as an Accountable Care Organization), would be likely to excessively limit competition in a particular community.
HHA. HHA is an abbreviation for Home Health Agency.
HHRG. See Home Health Resource Groups.
Hierarchical Condition Categories (HCCs). Hierarchical Condition Categories (HCCs) is a risk adjustment system developed by the Centers for Medicare and Medicaid System to pay Medicare Advantage plans that is now also being used in many of the payment models being implemented by CMS, such as the Medicare Shared Savings Program. The HCC system uses information about the diagnoses reported on claims forms for an individual patient during the preceding year in order to calculate a single numeric “risk score” for that patient. These risk scores are averaged across all of the patients associated with a clinician or health plan to determine the Risk Adjustment Factor (RAF) for that group of patients. Then the total spending during the year for a group of patients is divided by their RAF score to determine the risk-adjusted spending.
The HCC system is a regression-based risk adjustment system; CMS changes the weights for individual conditions significantly from year to year based on which factors achieve the best results in regression-based predictions of actual spending in the most recent year, not based on changes in clinical evidence about what patients need. CMS also implements HCCs as a prospective risk adjustment system that does not consider any health problems that occur during the performance year in determining the risk score for a patient; only diagnosis codes for health problems that occurred prior to the current year are considered. Moreover, the HCC system explicitly gives zero weight to many acute conditions, even though these conditions would likely result in a need for services during the year in which they occurred and could also affect service needs in the subsequent year. The HCC system uses only diagnosis information from claims data, and it does not consider many factors other than health conditions that can affect patient needs.
HMO (Health Maintenance Organization). A Health Maintenance Organization (HMO) is an entity that accepts a fixed premium or capitation payment for individuals enrolled in the HMO and takes responsibility for delivering or arranging for all of the covered healthcare services for those individuals through a defined group or network of clinicians. Typically an HMO requires that a patient have a referral from a primary care physician in the HMO before the patient can receive a non-emergency service from a specialist in the network, in contrast to a Preferred Clinician Organization (PPO) in which the patient can obtain most services from specialists in the PPO network without a referral or prior approval.
Network Model HMO. A network model HMO is the most common form of HMO. It is usually created by a health insurance plan contracting with multiple physician practices and hospitals to serve as the HMO clinicians. In a network model HMO, the HMO does not directly employ any of those clinicians.
Staff Model HMO. In a staff model HMO, a physician group serves as the HMO and takes the payment directly from the patient, rather than contracting through a separate health insurance plan. In a staff model HMO, most of the physicians are employed by the HMO.
Home Health Prospective Payment System (HH PPS). The Home Health Prospective Payment System (HH PPS) is the system Medicare uses to pay Home Health Agencies (HHAs). Home health agencies are paid with a single payment to cover all of the services that are delivered during a 60-day “episode.” Since different patients will need different amounts of service within a 60-day period, patients are assigned to one of 153 Home Health Resource Groups (HHRGs) based on their health problems, functional status, and number of home health visits provided. The Home Health Agency’s payment for a patient is based on the HHRG assigned. Different HHRGs are assigned in some cases if the patient is receiving the first or second episode of services or the third or subsequent episode, which means that the payment may differ for the same services depending on how long the patient has been receiving services. Different HHAs also receive different payment amounts for the same HHRG based on a geographic adjustment factor. The HHA can receive an additional Outlier Payment if the patient requires unusually costly services, and the HHA is paid on a per-visit basis if the patient receives fewer than 5 visits.
Home Health Resource Groups (HHRG). Home Health Resource Groups is a categorical risk adjustment system used in the Medicare Home Health Prospective Payment System (HH PPS). Patients are assigned to one of 153 Home Health Resource Groups (HHRGs) based on their health problems, functional status, and number of home health visits provided.
Hospice Services Payment. In the Medicare program, a hospice agency is paid a flat daily rate for each day that a beneficiary is enrolled in the hospice program. There are four different payment levels, depending on the type of care being provided – Routine Home Care (RHC), Continuous Home Care (CHC), Inpatient Respite Care (IRC), and General Inpatient Care (GIC). The payment rate for an individual patient is also adjusted by a geographic adjustment factor based on the location of the patient (not the location of the hospice agency, unlike the geographic adjustments for other clinicians).
Hospice payment is a form of capitation payment, since a fixed payment is made per beneficiary per day (at the RHC rate) regardless of how many services are provided on a given day (or whether any services are provided at all on a given day). A higher payment is only made if a service is provided which qualifies for the CHC, IRC, or GIC payment levels (and this typically only happens on a very small proportion of the days a patient is in hospice care). Hospice payment is also a bundled payment, since the payment is intended to cover a range of services that would otherwise be paid for separately under other Medicare payment programs, including home health services, drugs, physical, occupational, and speech therapy, and inpatient care. Moreover, the hospice payment is a prospective bundle, since after a Medicare beneficiary enrolls in hospice, clinicians are no longer eligible to receive direct payments from Medicare for delivering these kinds of services to the patient (if they are related to the hospice diagnosis) and any payments for those services must come through the hospice agency from the hospice payment.
Hospital-Acquired Condition (HAC). The Deficit Reduction Act of 2005 required CMS to develop a list of hospital-acquired conditions that (a) are high cost or high volume or both, (b) result in the assignment of a case to a DRG that has a higher payment when the hospital-acquired condition is present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence‐based guidelines. Since 2008, these conditions can no longer be used in determining the DRG for a hospital admission unless there is a specific indication that the condition was “present on admission.” In some cases, this can cause the hospital to receive a lower payment than it might otherwise, but if additional complications resulted from the hospital-acquired condition, these complications can still result in an increased payment to the hospital. The current list of Hospital-Acquired Conditions includes:
- Foreign Object Retained After Surgery
- Air Embolism
- Blood Incompatibility
- Stage III and IV Pressure Ulcers
- Falls and Trauma
- Manifestations of Poor Glycemic Control
- Catheter-Associated Urinary Tract Infection (UTI)
- Vascular Catheter-Associated Infection
- Surgical Site Infection, Mediastinitis, Following Coronary Artery Bypass Graft (CABG):
- Surgical Site Infection Following Bariatric Surgery for Obesity
- Surgical Site Infection Following Certain Orthopedic Procedures
- Surgical Site Infection Following Cardiac Implantable Electronic Device (CIED)
- Deep Vein Thrombosis (DVT)/Pulmonary Embolism (PE) Following Certain Orthopedic Procedures:
- Iatrogenic Pneumothorax with Venous Catheterization
Hospital-Acquired Condition Reduction Program. Beginning in October 2014, CMS began implementing the Hospital-Acquired Condition Reduction Program, which reduces Medicare payments for inpatient stays in hospitals that have the highest rates of certain hospital-acquired conditions (HACs). The worst performing quartile of hospitals is identified by calculating a Total HAC score based on the hospital’s performance on three quality measures (Patient Safety Indicator 90 composite, central-line associated bloodstream infection, and catheter associated urinary tract infection). If a hospital has a Total HAC score above the 75th percentile of the distribution of Total HAC scores for all hospitals, the hospital’s payments are reduced by 1% for all of its patients.
Hospital Readmissions Reduction Program. Since October 2012, CMS has reduced payments to a hospital for its inpatient admissions if the hospital is determined to have “excess” readmissions. A readmission is an admission to the same or another acute care hospital within 30 days of discharge, other than for specifically planned readmissions such as for chemotherapy or rehabilitation, and a hospital has “excess readmissions” if its rate of readmissions is higher than an expected readmission rate. Initially, the program measured readmissions only for Medicare patients with diagnoses of acute myocardial infarction (heart attack), heart failure, or pneumonia. If the hospital is determined to have excess readmissions, the payments for all of its patients are reduced, not just those in the categories where readmissions were high. The maximum penalty was initially capped at 1 percent and can now be as high as 3 percent per year. (The hospital is still paid for the readmissions themselves; the penalty is a reduction in payment for all admissions, including the readmissions.)
Hospital Value-Based Purchasing Program (Hospital VBP). Since October 2012, CMS has modified payments to hospitals based on their performance on a series of quality and spending measures under the Medicare Hospital Value-Based Purchasing (Hospital VBP) Program. There are three steps in the VBP:
- First, all DRG payments to all hospitals are reduced across-the-board by a percentage that increases each year until it reaches 2% in 2017 and subsequent years.
- Second, each hospital’s performance on a series of quality and spending measures is determined and compared to its own previous performance and the current performance of other hospitals to calculate a score for the hospital.
- Third, each hospital’s score is converted (using a “linear exchange function”) into a percentage increase that is then applied to its DRG payment.
The net effect of the reductions in the first step and the increases in the third step is that some hospitals will see a net increase in their payments and some hospitals will see a net reduction in their payments through the Hospital VBP program, in addition to any increases or decreases they experience through other changes in Medicare payments.
Hospital Wage Index (HWI). The Hospital Wage Index (HWI) is a Geographic Adjustment Factor used by Medicare to adjust payments to hospitals, skilled nursing facilities, and other clinicians to account for differences in the wage rates in their local labor markets. The hospital wage index for a labor market area is calculated by taking the average hourly wage (AHW) paid to full-time, part-time, and contract workers by all hospitals in the labor market area that are paid through the Medicare IPPS, and dividing that average by the AHW for all IPPS hospitals nationwide. The HWI for each labor market area is then used to adjust the payment rate for each patient discharged from a hospital in that labor market area, so that hospitals in areas with higher average wage rates receive higher payments from Medicare.
Back to top
I
IBNR (Incurred But Not Reported). If clinicians have delivered services but have not yet submitted claims for those services to the payer who is obligated to pay the claims, then the claims are described as “Incurred But Not Reported (IBNR).” If a payer has agreed to pay claims for services rendered from a fixed premium (or if a clinician has agreed to accept a bundled payment and pay other clinicians for specific types of services they render), then IBNR claims represent a liability that the payer or clinician is obligated to pay, but the payer/clinician does not know the amount of the liability until the claims are actually filed. Consequently, in order for the payer (or the clinician managing a multi-clinician bundled payment) to know whether its expenses will be lower or higher than its revenues, it needs a way to estimate IBNR.
ICD-9 CM. ICD-9 is the International Classification of Diseases, 9th Edition, Clinical Modification. It is the official national mechanism in the United States for coding diagnoses on claims forms until a transition is made to ICD-10. Alphanumeric codes are assigned to diseases as well as some of the causes of health problems. Examples of ICD-9-CM diagnosis codes include:
- 162.5 Malignant Neoplasm of Lower Lobe, Bronchus or Lung
- 428.32 Chronic Diastolic Heart Failure
- E916 Struck accidentally by falling object ICD-9-CM also defines procedure codes that are used by hospitals for billing purposes. Examples include:
- 37.51 Heart Transplantation
- 84.17 Amputation of leg above knee
ICD-10-CM. ICD-10 is the International Classification of Diseases, 10th Edition, Clinical Modification. It has more detailed coding for some diagnoses than ICD-9- CM, and it only contains diagnosis codes; procedure codes are included in ICD-10-PCS. Examples of ICD- 10-CM diagnosis codes include:
- C34.31 Malignant Neoplasm of Lower Lobe, Right Bronchus or Lung
- 150.32 Chronic Diastolic Health Failure
ICD-10-PCS. ICD-10-PCS contains an updated set of the procedure codes that were previously included as Volume III of ICD-9-CM. These procedure codes are used by hospitals for billing purposes.
IME. See Indirect Medical Education Adjustment
Improvement. In a payment model where the amount of payment is based on performance on one or more measures of quality or spending, “improvement” is used to refer to the change in the clinician’s level of performance in a performance period compared to the clinician’s performance in a baseline period. In contrast, “achievement” is a measure of how the clinician’s level of performance compares to a benchmark that is established based on what other clinicians have achieved or can achieve. Since a clinician that failed to meet an achievement threshold may still have significantly improved its performance, many pay-for-performance systems are based on both achievement and improvement.
Improvement Threshold. In a pay for performance system, an improvement threshold is a level of improvement that must be reached in order to qualify for a payment or an adjustment in payment.
Independent Practice Association (IPA). An Independent Practice Association is an organization consisting of two or more independent physician practices that work jointly in some way. Some IPAs accept payment contracts on behalf of their members, others provide mechanisms for multiple practices to share infrastructure costs or staff that would otherwise not be affordable for small practices.
Indirect Medical Education (IME) Adjustment. Under the Medicare Inpatient Prospective Payment System, hospitals that have medical residents in approved graduate medical education (GME) programs receive higher payments for each Medicare patient who receives care in the hospital. The Indirect Medical Education (IME) adjustment increases the DRG payment amount for each patient by a specific percentage called the IME adjustment factor. The size of the adjustment factor is based on the ratio of the number of medical residents to the number of beds in the hospital.
Infrastructure. “Infrastructure” is a generic term used to describe systems and services that a clinician needs to have in order to deliver quality care to patients. The term is used to refer to fixed assets such as computer equipment, software systems such as electronic health records or data analysis software.
Infrastructure Payment. An infrastructure payment is a payment that is specifically designed to support the costs of “infrastructure” that a clinician uses to deliver or manage care. In some cases, payer have required that the payment only be used for specific kinds of “infrastructure,” whereas in others, the payment is made because of a recognition that a clinician needs adequate payment to support the infrastructure required to deliver high-quality care but no restrictions are placed on how the clinician can spend the payment.
Innovation Center. See Center for Medicare and Medicaid Innovation.
In-Office Ancillary Services Exception. The In-Office Ancillary Services Exception (IOASE) is a provision of the federal Stark Law that exempts physician practices from the general prohibition on referral to clinicians in which physicians have a financial interest. It applies in the case of ancillary services delivered in a physician’s office or practice site by the physician, by another physician who is a member of the same practice, or by an individual supervised by the physician
Inpatient Prospective Payment System (IPPS). The Inpatient Prospective Payment System (IPPS) is the payment system used by Medicare to pay most large acute care hospitals for inpatient hospitalizations. (Critical Access Hospitals are paid on a cost-based retrospective reimbursement system.) In the IPPS, a hospital is paid a case rate for each patient, i.e., it receives a single payment for the patient’s entire stay. The case rate is determined by taking a conversion factor called the base rate, adjusting it for geographic cost differences using the Hospital Wage Index for the area where the hospital is located, and then multiplying the adjusted rate by on the weight of the MS- DRG (Medicare Severity Diagnosis Related Group) to which the patient is assigned based on the diagnoses recorded for the patient and the procedures performed.
The case rate is further adjusted through three other programs:
- Under the Hospital Readmissions Reduction Program, the hospital’s payments for all patients are reduced if the hospital’s readmission rates for specific kinds of conditions are higher than a benchmark level;
- Under the Hospital-Acquired Condition Reduction Program, the DRG for a patient is revised to exclude consideration of certain hospital-acquired conditions that were not present when the patient was admitted to the hospital, and if the hospital has a high rate of hospital-acquired conditions, its payments for all patients are reduced by 1%.
- Under the Hospital Value-Based Purchasing Program, the hospital’s payments for all patients are adjusted up or down using a Value-Based Incentive.
Payment Adjustment that is calculated by evaluating the hospital’s performance relative to benchmarks on several measures of the quality of care in the hospital and the total cost of services for the hospital’s patients.
Selected hospitals receive still further adjustments to their payments:
- teaching hospitals receive an additional Indirect Medical Education (IME) payment
- hospitals with large numbers of low-income patients receive an additional Disproportionate Share (DSH) payment.
- rural hospitals designated as Sole Community Hospitals receive the greater of the IPPS case rate payment or a payment based on their costs in a base year trended forward to the current year and adjusted for the hospitals’ current case mix.
- some hospitals with low volumes of patients receive a Low-Volume Payment Adjustment.
A hospital can receive an additional Outlier Payment for an individual patient if the patient requires unusually costly services; it can receive an additional payment it has used certain new technologies for care of the patient; and it can receive additional payments for bad debts resulting from patients’ non-payment of cost-sharing amounts. If a patient has a very short stay and is transferred to another acute care hospital or to post-acute care, the hospital will be paid on a per diem basis (i.e., based on the number of days the patient was in the hospital) rather than based on the case rate it would otherwise qualify for based on the patient’s characteristics and the services delivered.
Inpatient Psychiatric Facility Prospective Payment System (IPF-PPS). The Inpatient Psychiatric Facility Prospective Payment System (IPF PPS) is the system Medicare uses to pay Inpatient Psychiatric Facilities. In contrast to the Inpatient Prospective Payment System, which pays an acute care hospital a single case rate (the DRG payment) regardless of the length of stay, an Inpatient Psychiatric Facility (IPF) receives an additional payment for each day the patient stays in the hospital, i.e., the hospital is paid on a per diem basis. The amount of payment for each day decreases the longer the patient is in the hospital, but the total payment still increases the longer the patient stays. The per diem amount is also adjusted based on the patient’s characteristics, the nature of the facility, and the location of the facility. The hospital receives additional payments if electroconvulsive therapies are delivered and the hospital can receive an outlier payment if the patient requires unusually expensive services.
Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS). The Inpatient Rehabilitation Facility Prospective Payment System (IRF PPS) is the system used by Medicare to pay inpatient rehabilitation facilities (IRFs). Similar to the Inpatient Prospective Payment System for acute care hospitals, the IRF PPS pays IRFs a case rate for each patient, i.e., a single payment for the patient’s entire stay. The case rate is determined by taking a conversion factor called the base rate, adjusting it for geographic cost differences based on where the IRF is located, and then multiplying the adjusted rate by the weight of the Case-Mix Group (CMG) to which the patient is assigned. There are 92 different CMG categories, and the patient is assigned to a category based on the diagnosis that led to the need for rehabilitation, their comorbidities, their age, and their functional and cognitive status. The facility can receive an additional Outlier Payment if the patient requires unusually costly services. For patients who have short stays, a lower payment is made.
Intermediate Outcome Measure. An intermediate outcome measure is a form of quality measure that determines whether specific kinds of results were achieved from healthcare services that are viewed as valuable solely or primarily because they have been shown to lead to other desirable outcomes. For example, a low hemoglobin A1c (HbA1c) level for a patient is an intermediate outcome measure that is viewed as desirable because it reduces the risk of other complications of diabetes, such as blindness and amputations. Compare the definitions of Process Measure and Outcome Measure.
Internal Cost Savings. Internal cost savings is the amount by which a clinician’s cost decreases for the services delivered in return for a particular payment if a different mix of services is used within the payment bundle or if changes are made in the way individual services are delivered. If the clinician achieves higher internal cost savings in delivering services for the same payment amount, its margin will increase. A payer will not directly benefit from a clinician’s internal cost savings unless the payment agreement explicitly provides for a way to reduce the payer’s payment. For example, in Model 1 of the Bundled Payments for Care Improvement Initiative, CMS requires a hospital to accept a lower Medicare payment in return for the ability to gain-share internal cost savings with physicians.
IPA. See Independent Practice Association.
IPF. IPF is an abbreviation for Inpatient Psychiatric Facility. See Inpatient Psychiatric Facility Prospective Payment System.
IPPS. See Inpatient Prospective Payment System.
Back to top
J
J-Code. A J-Code is a subset of the Level II codes that CMS creates and maintains as part of the Healthcare Common Procedure Coding System (HCPCS). Jcodes define specific types of drugs that Medicare will pay physicians to administer.
Back to top
L
Lemon-Dropping. Lemon-dropping is a colloquial term used to describe a situation in which a payer or healthcare clinician avoids insuring or caring for a patient for whom the cost of services is expected to exceed the payment for those services or the premium received for their health insurance. See also
Cherry-Picking.
Length of Stay (LOS). Length of stay is the amount of time that a patient spends in a hospital or other facility in order to receive a particular service or group of services.
Limiting Charge. In the Medicare program, the Limiting Charge is the maximum amount that a physician can charge a Medicare Beneficiary for a service if the physician is a Non-Participating Physician. A nonparticipating physician is paid 95% of the Medicare approved amount for participating physicians, the Limiting Charge is 115% of that amount, and the difference between Medicare’s payment to the physician and the Limiting Charge can be Balance Billed to the patient.
Linear Exchange Function. A “linear exchange function” is a formula for translating a clinician’s performance score on one or more measures of quality or spending into a change in the clinician’s payment. In the Medicare Hospital Value-Based Purchasing Program, hospitals are assigned a Total Performance Score between 0 and 100 based on the hospital’s performance on a series of different measures, and then a linear exchange function is used to convert the Total Performance Score into the Value-Based Incentive Payment Adjustment.
Long-Term Care Hospital Prospective Payment System (LTCH PPS). The Long-Term Care Hospital Prospective Payment System is the payment system Medicare uses to pay long-term care hospitals. Similar to the Inpatient Prospective Payment System for acute care hospitals, the LTCH PPS pays LTCHs a case rate for each patient, i.e., a single payment for the patient’s entire stay. The case rate is determined by taking a conversion factor called the base rate, adjusting it for geographic cost differences based on where the LTCH is located, and then multiplying the adjusted rate by the weight of the MS-LTC-DRG (Medicare Severity Long- Term Care Diagnosis Related Group) to which the patient is assigned. The facility can receive an additional Outlier Payment if the patient requires unusually costly services. For patients who have short stays, an alternative methodology is used to determine the payment based on actual costs and length of stay.
Look-Back Period. A look-back period is a prior period of time for which data are collected to compute a measure. For example, a quality measure may be based on actions taken by a clinician or a patient’s test results that occurred during a specific number of months prior to the date the measure is calculated. Attribution methodologies typically include a look-back period for determining which clinician had the largest number of visits or delivered the largest number of services to a patient.
LOS. See Length of Stay.
Low-Volume Hospital Payment Adjustment. In the Medicare Low-Volume Hospital Payment Adjustment program, certain small hospitals in rural areas have received higher payments than they would otherwise receive. This program was created to compensate for the fact that all else being equal, a hospital that delivers a particular type of service to a small number of patients will have higher average costs per patient than hospitals that treat larger numbers of patients because the hospital’s fixed costs of delivering the service will have to be allocated to a smaller number of patients.
Back to top
M
Managed Care Organization (MCO). In the Medicaid program, states are permitted to contract with Managed Care Organizations to pay clinicians for services to Medicaid recipients rather than the state paying the clinicians directly.
Margin. The difference between total revenues and expenses for an organization or service line. See also Contribution Margin.
Market Basket. In order to update payment rates from year to year, the Office of the Actuary within the Centers for Medicare and Medicaid Services (CMS) calculates a “market basket” for each of its payment systems that is designed to measure the price changes each type of clinician (hospitals, skilled nursing facilities, home health agencies, etc.) experiences for the supplies and services it purchases. Market basket levels are released quarterly.
MCC. MCC is an abbreviation for Major Complications and Comorbidities that is used in the DRG system. See Diagnosis Related Groups.
MCO. See Managed Care Organization.
Measure Weight. In a payment model that defines a performance score based on a clinician’s performance on multiple measures, each measure is assigned a measure weight to specify how performance on that measure will be adjusted in order to combine it with performance on other measures in calculating an overall performance score. A measure weight is partly an indication of a measure’s relative importance in assessing overall performance (since a measure with a higher measure weight will have a greater impact on the total performance score) and partly a method of adjusting for differences in the measurement scales for different measures (e.g., if the performance level on one measure can vary from 0 to 10 and the performance level on another measure can vary from 0 to 100, then if the measures are viewed as equally important, the first measure will need to have a weight that is 10 times the weight for the second measure).
Medical Home. A medical home is a generic term used to describe a physician practice which operates in ways consistent with one or more of the principles of the Patient-Centered Medical Home. Although a “medical home” was originally intended to apply to primary care practices, it has also been used to refer to specialty practices that provide care to patients with a particular health problem in ways that are consistent with one or more of the principles of the Patient-Centered Medical Home.
Medical Home Payment. A wide range of different “medical home payment models” have been created by payers to assist or encourage primary care practices, and in some cases specialty physician practices, to deliver care consistent with one or more of the principles of the Patient-Centered Medical Home. These payment models have generally been structured in one of the following ways.
- Additional or increased payment based on accreditation or certification. In this payment model, the physician practice receives additional payment if it is accredited or certified by the payer or by an independent organization as meeting specific standards for the way it delivers care. Different mechanisms are used to deliver the additional payment; in some payment models, the practice receives higher payments for existing billing codes (typically evaluation and management service codes), while in other payment models, the practice receives a PMPM payment for each of the payer’s patients.
- Payment for infrastructure. In this payment model, the physician practice receives payment to cover all or part of the cost of “infrastructure” that the practice uses to deliver care to patients. For example, the practice might receive payment to cover all or part of the costs of purchasing and installing an electronic medical record system.
- New payments for specific services. In this payment model, the physician practice receives payment designed to support specific services, such as hiring a nurse care manager to provide services to patients with chronic diseases. Different mechanisms are used to deliver the additional payment: in some systems, the practice is permitted to bill for services that would otherwise not be eligible for payment (e.g., the practice is permitted to bill for time spent by a nurse in providing education to chronic disease patients) and in other systems, the practice receives a PMPM payment but it is required to use the payment on the specified services. Some payers, instead of providing payments to a practice to hire staff such as care managers, have hired the staff directly on the payer’s payroll and assigned them to work at the physician practice office.
- New, flexible payments. In this payment model, the physician practice receives a payment, such as a PMPM payment, in addition to existing fee-for-service or other payments it receives, with the flexibility to use the payment in a wide range of ways.
- Pay-for-performance payments. In this payment model, the physician practice receives additional payment if it achieves specific performance levels on measures of quality or spending.
- Shared savings payments. In this payment model, the physician practice receives additional payment based on a portion of savings that the payer determines it has achieved as a result of improved delivery of services.
- Combination payments. A combination of one or more of the above mechanisms can also be used. For example, in the Medicare Comprehensive Primary Care Initiative, in addition to current payments under the Medicare Physician Fee Schedule, participating primary care practices receive a risk-adjusted PMPM payment that can be used for a wide range of services, and they can also receive a shared savings payment if spending for all of the patients in the all of the participating practices in the state or region is lower than spending for patients in non-participating practices.
Medical Loss Ratio (MLR). The “medical loss ratio” is a term used in health insurance that means the total amount a health plan spends on payments for healthcare services divided by the total premium revenues received to cover those payments. The medical loss ratio is typically described as a percentage, the ratio must be lower than 100% in order for the insurance plan to remain solvent, since administrative expenses and profits are not included in the “medical loss,” and a health plan must also retain some portion of premiums as a reserve against variations in the medical loss ratio. The Affordable Care Act established minimum thresholds for the Medical Loss Ratios of commercial insurance plans.
Although not typically used in the context of payment models, the concept of Medical Loss Ratio is equally applicable to payments, since the entity that manages a multi-clinician bundled payment must ensure that the payments to all clinicians are lower than the amount of payment, while also leaving enough funds to cover any administrative costs associated with managing the payment and to provide a reserve for variations in the need for services within the payment amount. Moreover, if a payer begins using more accountable payment models to pay clinicians, the payer will be transferring some portion of its administrative costs and risks to the clinicians, which will affect medical loss ratios for both the payer and the clinician and require different judgments about whether those ratios are too high or low.
Medical Neighborhood. A “medical neighborhood” is a set of specialists and other clinicians who provide healthcare services to the patients who are part of a primary care medical home.
Medically Unlikely Edit (MUE). A Medically Unlikely Edit is part of the National Correct Coding Initiative and defines combinations of services or types of services that are unlikely to occur and may indicate an error in coding or potential fraudulent billing.
Medicare Economic Index (MEI). The Medicare Economic Index (MEI) is a method of measuring inflation in the cost of operating a medical practice. It is conceptually similar to the Consumer Price Index and the Producer Price Index used for other industries, but it is based on the cost of items that are relevant to medical practices. CMS calculates and publishes the MEI on a quarterly basis.
Medicare Shared Savings Program (MSSP). The Medicare Shared Savings Program is a payment program established by the Affordable Care Act (in Section 1899 of the Social Security Act) that clinicians can voluntarily choose to participate in if they meet the qualifications for an Accountable Care Organization (ACO) established in the statute and in regulations promulgated by CMS. Although the Shared Savings Program authorizes the use of shared savings as one method of payment to ACOs, it also authorized the use of “Other Payment Models,” including a partial capitation model. See Shared Savings for more information.
Medicare Spending Per Beneficiary (MSPB). Medicare Spending Per Beneficiary is one of the performance measures used to determine the Value-Based Incentive Payment Adjustment for a hospital and to determine the Value-Based Payment Modifier for a physician practice. Total Medicare Part A and Part B spending (i.e., payments for institutional and professional services, but not for prescription drugs) are tabulated for a hospitalized patient from the point 3 days prior to hospital admission through the point 30 days after discharge from the hospital, and then the sum is risk adjusted for patient characteristics using the HCC risk adjustment system and further adjusted using standardized payments.
In the Value-Based Incentive Payment for a hospital, the Medicare Spending Per Beneficiary measure is calculated for all patients discharged from the hospital, and then the average is compared to the average for the measure for all hospitals. In the Value-Based Payment Modifier for physician practices, a hospitalization is attributed to the physician group that provided the plurality of professional services during the hospital stay (as measured by the total payments for the services), and the MSPB is calculated for that hospitalization. The average of the MSPB measures for all patients attributed to the physician practice is then compared to the average for all physician practices after adjusting for the mix of specialties in the practice.
MEI. See Medicare Economic Index.
Merit-Based Incentive Payment System (MIPS). The Merit-Based Incentive Payment System is a Medicare pay-for-performance system for physicians created by the Medicare Access and CHIP Reauthorization Act (MACRA) that is to be implemented beginning in 2019. It consolidates several existing Medicare pay-for-performance programs – the EHR Incentive program, the Physician Quality Reporting System, and the Value-Based Payment Modifier – into a single pay-for-performance program that will be based on four categories of performance measures: quality, resource use, clinical practice improvement activities, and meaningful use of certified EHR technology. Physicians will receive either increases or decreases in their payments under the Physician Fee Schedule based on their performance in the MIPS program; because the program is supposed to be budget-neutral, the magnitude of any increases received by physicians who qualify for increases will depend on the number of physicians receiving decreases in payments and the magnitude of those reductions.
Physicians participating in Alternative Payment Models that meet the criteria defined in MACRA are exempt from the MIPS payment adjustments and also receive a bonus payment equal to 5% of their Medicare payments under the Physician Fee Schedule.
Minimum Loss Rate. In a Shared Savings program, the minimum loss rate is the minimum amount that the actual spending must be above the benchmark in order for the clinician to be obligated to pay the payer a share of the increased spending the payer has incurred. A minimum loss rate is typically used to avoid a clinician having to make payments to a payer based simply on random variation in spending. For more information, see Minimum Savings Rate.
Minimum Savings Rate (MSR). In a Shared Savings program, the minimum savings rate (MSR) is the minimum amount that the actual spending must be below the benchmark in order for the clinician to qualify for a shared saving payment. A minimum savings rate can be used for two separate purposes:
- to avoid the payer making a shared savings payment to a clinician based simply on random variation in spending. For example, in the Medicare Shared Savings Program, higher minimum savings rates are used for Accountable Care Organizations with fewer attributed beneficiaries, since the likelihood of random variation in patient needs causing reductions in spending is higher when there are fewer patients.
- to increase the proportion of savings retained by the payer when small amounts of savings are achieved. In a first dollar shared savings model, the clinician receives a share of all savings, including the savings in the minimum savings rate, but otherwise, the payer retains the savings in the minimum savings rate and then shares any additional savings above that.
MIPS. See Merit-Based Incentive Payment.
MLR. MLR is an abbreviation for Medical Loss Ratio but also sometimes refers to a Minimum Loss Rate.
Modifier. A modifier is an additional code appended to a billing code to communicate additional information about the circumstances in which the service was delivered. The modifier is often used to indicate that the payment for the service should be different than what is paid for the unmodified code. For example, Modifier 33 is added to CPT codes to indicate that a service was preventative in nature and that patient cost-sharing does not apply.
MS-DRG (Medicare Severity Diagnosis Related Groups). MS-DRGs are the version of DRGs used in the Medicare Inpatient Prospective Payment System. In the current MS-DRG system, there are 751 different MSDRGs to which an inpatient admission can be assigned.
MS-LTC-DRGs (Medicare Severity Long-Term Care Diagnosis Related Groups). MS-LTC-DRGs are used to determine payments to Long-Term Care Hospitals in the Medicare Long-Term Care Hospital Prospective Payment System. They have the same definitions and structure as MS-DRGs, but the payment weights are different in order to reflect the differences in costs for patients in long-term care hospitals instead of acute care hospitals. See Long-Term Care Hospital Prospective Payment System.
MSPB. See Medicare Spending Per Beneficiary.
MSR. See Minimum Savings Rate.
MSSP. See Medicare Shared Savings Program.
Multi-Clinician Bundle. A multi-clinician bundle is a bundled payment that includes services delivered by multiple clinicians. Multi-clinician bundles are more complicated to administer than single-clinician bundles because an entity needs to be defined to receive the payment on behalf of all of the clinicians and a method is needed to allocate the bundled payment among the individual clinicians. One approach is to treat the bundled payment as a budget, allow each clinician to continue billing and being paid for their individual services under fee-for-service models, and then retrospectively reconciling the bundled payment budget after all of the services have been delivered. An alternative is to treat the bundled payment as a prospective payment, designate one clinician or an entity jointly formed by all of the clinicians to accept the bundled payment, and then they develop a mechanism for allocating the bundled payment among the individual clinicians.
Musculoskeletal Medical Home. A “musculoskeletal medical home” is a clinician such as an orthopedic physician practice that delivers care to individuals with musculoskeletal problems (such as osteoarthritis of the joints) in ways that are consistent with one or more of the principles of the Patient-Centered Medical Home.
Back to top
N
Narrow Network. A narrow network is a network of clinicians that is smaller than the network available to a patient under a different insurance plan or payment model. The choice of which clinicians are in the narrow network may be based on their willingness to accept lower payments, their scores on measures of quality or cost, their willingness or ability to coordinate care, or other factors.
National Correct Coding Initiative (NCCI). The National Correct Coding Initiative is a program operated by CMS that is designed to avoid payment for inappropriate or duplicative services. NCCI defines a series of rules that are applied when a payer processes healthcare claims in order to identify codes that should generally not be billed at the same time or combinations of codes that are not consistent with typical or appropriate patterns of care.
NCCI. See National Correct Coding Initiative.
Net Payment Reconciliation Amount. In a retrospective reconciliation process, the Net Payment Reconciliation Amount is the amount of money that must be transferred between a payer and a clinician to ensure that the total payment is equal to the agreed-upon amount.
Network. In healthcare delivery and payment, a network consists of two or more clinicians who will deliver services in return for agreed-upon payment and cost-sharing amounts for patients who are covered under a particular health insurance plan or who are receiving services as part of a bundled or global payment.
Network Adequacy. The adequacy of a network is the ability of the clinicians in the network to achieve certain standards in the way they deliver services to the patients who are being required or encouraged to use the network. The most basic standard of adequacy is to have at least one clinician in the network who can deliver each service that a patient could potentially need under the insurance plan or payment. However, adequacy requirements can also include the distance a patient must travel to receive care from a clinician who can deliver the service the patient needs, the quality of care the clinicians in the network deliver, etc.
Next Generation ACO. See Accountable Care Organization.
Non-Covered Service. A non-covered service is a healthcare service that a patient’s health insurance plan will not pay any healthcare clinician to deliver. If the patient wants the service, they would need to pay a clinician for the service using the patient’s own funds.
Non-PAR. See Non-Participating Physician.
Non-Participating Physician. A physician or other clinician who has not agreed to accept Assignment for all services delivered to Medicare beneficiaries. Non- Participating Physicians may choose to accept assignment on a service-by-service basis. See Assignment.
Non-Preferred Clinician. A clinician that is not designated as a Preferred Clinician. See Preferred Clinician.
Back to top
O
OCM. See Oncology Care Model
Oncology Care Model (OCM). The Oncology Care Model (OCM) is a demonstration project announced by the Center for Medicare and Medicaid Innovation in 2015 that is intended to improve the quality and reduce the cost of care for cancer patients. As proposed, OCM would initially be a combination of a supplemental capitation payment and either an upside-only shared savings model or a shared-risk model.
- An oncology practice participating in the program would be able to bill for a new $160 payment each month for a six-month “episode” following the initiation of chemotherapy for a patient, regardless of how many months during the six-month period the patient continues to receive chemotherapy. This payment would be in addition to all existing fee-for-service payments. If the patient continues to receive chemotherapy more than 6 months after the initial chemotherapy treatment, then the oncology practice could again bill for a $160 monthly payment for another six-month episode.
- If the oncology practice chooses the upside-only shared savings option, it would be eligible to receive an additional payment if the average total Medicare spending for the practice’s patients (on all services, not just oncology services) during the six-month episodes is more than 4% lower than an expected level of spending. The expected level of spending would be based on the average spending for the practice’s patients during 6-month episodes during a baseline period, trended forwarded and risk-adjusted using a methodology CMMI has not yet announced. The amount of the payment to the practice would be based on the difference between the actual spending and 96% of expected spending and also on the practice’s performance on a series of quality measures. Although the practice would not be liable for any payments to CMS if spending levels increased, it would be terminated from the OCM program if spending was not reduced by at least the 4% target level.
- If the oncology practice chooses the shared-risk option, it would be eligible to receive an additional payment if actual spending during the episodes averaged at least 2.75% below expected spending levels, but it would also be liable to pay CMMI a portion of any spending that is more than 2.75% of the expected spending level.
Oncology Medical Home. An “oncology medical home” is a general term being used to describe an oncology practice that delivers care to individuals with cancer in ways that are consistent with one or more of the principles of the Patient-Centered Medical Home. A key issue that oncology medical homes are seeking to address is to better manage complications of chemotherapy to reduce the rate at which their patients make emergency room visits and are hospitalized for complications.
OOP. See Out-of-Pocket Maximum.
OPPS. See Outpatient Prospective Payment System.
Outcome Measure. An outcome measure is a form of quality measure that assesses the result of healthcare services in terms of patient health, quality of life, or functionality. See also Intermediate Outcome Measure and Process Measure.
Outlier Patient. An outlier patient is a patient who receives or requires a much larger number of services or much more expensive services than other patients. See Exclusion, Truncation, Winsorization, and Outlier Payment for methods by which payment models adjust payments for outlier patients.
Outlier Payment. An outlier payment is an additional payment made to a clinician to cover all or part of the additional costs of services delivered to an outlier patient. For example, in the Medicare Inpatient Prospective Payment System, a hospital receives a payment for each patient based on the Diagnosis Related Group (DRG) to which the patient is assigned, but if the cost of treating a particular patient exceeds the DRG payment by a minimum amount, the hospital will receive an additional outlier payment from Medicare for that patient.
Out-of-Network. Out-of-network care is a healthcare service delivered by a clinician that is not part of the network of clinicians that a patient is being encouraged or required to use. Typically, a patient is expected to pay more (or to pay the full cost) if they receive a service from an out-of-network clinician.
Out-of-Pocket Maximum. In a health insurance plan, if the cumulative amount of cost-sharing payments (i.e., co-payments, co-insurance, and deductibles) paid by a patient for healthcare services during a year (or other period of time) reaches the out-of-pocket maximum or out-of-pocket limit, the health plan then pays 100% of the payments for services to clinicians for the remainder of the year (or whatever time period the maximum applies).
Outpatient Prospective Payment System (OPPS). The Outpatient Prospective Payment System (OPPS) is the payment system used by Medicare to pay most large acute care hospitals for outpatient services. Prior to 2000, Medicare paid for outpatient services based on hospitals’ costs. (Critical Access Hospitals are still paid on a cost-based retrospective reimbursement system for inpatient and outpatient services.) The OPPS bases payments on the same CPT and HCPCS codes that are used in the Physician Fee Schedule, but the payment amount is based on the Ambulatory Patient Classification (APC) to which the code is assigned. Moreover, if multiple services in the same Ambulatory Patient Classification are delivered at the same time, only one payment is made, so the OPPS is a “partial bundled” payment model. As in the Inpatient Prospective Payment System, the payment amount for the same service differs from hospital to hospital based on geographic adjustments using the Hospital Wage Index, and a hospital can receive an Outlier Payment for patients who required unusually costly services. Additional payments are made for services delivered in Sole Community Hospitals, cancer hospitals, and children’s hospitals and for use of new technologies.
In general, the payment rate for a service under the OPPS is higher than if the same service is delivered in a physician’s office (this is called a Site-of-Service Differential), but under the OPPS, services in the same APC will not receive separate payments if they are delivered at the same time, whereas if the services are delivered in a physician’s office, separate payments will be made for each service. As a result, it is difficult to directly compare the costs of services delivered in an outpatient hospital department to services delivered in physician offices without knowing what combination of services each uses to treat the same condition or deliver the same procedure.
Overuse. Overuse is the use of a particular service more often than is necessary or justified based on evidence about its effectiveness.
Back to top
P
PAC. The abbreviation PAC has been used to mean both “post-acute care” and “potentially avoidable complication.”
Partial Bundle. See Bundled Payment.
Partial Capitation. See Capitation.
Participating Physician. A physician who agrees to accept Medicare Physician Fee Schedule payments as payment in full for services delivered to Medicare beneficiaries. (This is described as “Accepting Assignment.”)
Pathway. See Clinical Pathway.
Patient-Centered Medical Home. A Patient-Centered Medical Home is a primary care practice that is structured and operated consistent with a set of principles jointly developed by the American Academy of Family Physicians (AAFP), the American Academy of Pediatrics (AAP), the American College of Physicians (ACP), and the American Osteopathic Association (AOA). The principles are:
- Personal physician - each patient has an ongoing relationship with a personal physician trained to provide first contact, continuous and comprehensive care.
- Physician directed medical practice – the personal physician leads a team of individuals at the practice level who collectively take responsibility for the ongoing care of patients.
- Whole person orientation – the personal physician is responsible for providing for all the patient’s healthcare needs or taking responsibility for appropriately arranging care with other qualified professionals. This includes care for all stages of life; acute care, chronic care, preventive services, and end of life care.
- Care is coordinated and/or integrated across all elements of the complex healthcare system (e.g., subspecialty care, hospitals, home health agencies, nursing homes) and the patient’s community (e.g., family, public and private community-based services). Care is facilitated by registries, information technology, health information exchange, and other means to assure that patients get the indicated care when and where they need and want it in a culturally and linguistically appropriate manner.
- Quality and safety are hallmarks of the medical home: Practices advocate for their patients to support the attainment of optimal, patient-centered outcomes that are defined by a care planning process driven by a compassionate, robust partnership between physicians, patients, and the patient’s family; evidence-based medicine and clinical decision-support tools guide decision making; physicians in the practice accept accountability for continuous quality improvement through voluntary engagement in performance measurement and improvement; patients actively participate in decision making and feedback is sought to ensure patients’ expectations are being met; information technology is utilized appropriately to support optimal patient care, performance measurement, patient education, and enhanced communication; practices go through a voluntary recognition process by an appropriate non-governmental entity to demonstrate that they have the capabilities to provide patient centered services consistent with the medical home model; and patients and families participate in quality improvement activities at the practice level.
- Enhanced access to care is available through systems such as open scheduling, expanded hours and new options for communication between patients, their personal physician, and practice staff.
- Payment appropriately recognizes the added value provided to patients who have a patient-centered medical home. The payment structure should be based on the following framework: It should reflect the value of physician and non-physician staff patient-centered care management work that falls outside of the face-to-face visit; it should pay for services associated with coordination of care both within a given practice and between consultants, ancillary clinicians, and community resources; it should support adoption and use of health information technology for quality improvement; it should support provision of enhanced communication access such as secure e-mail and telephone consultation; it should recognize the value of physician work associated with remote monitoring of clinical data using technology; it should allow for separate fee-for-service payments for face-to-face visits (payments for care management services that fall outside of the face-to-face visit, as described above, should not result in a reduction in the payments for face-to-face visits); it should recognize case mix differences in the patient population being treated within the practice; it should allow physicians to share in savings from reduced hospitalizations associated with physician-guided care management in the office setting; and it should allow for additional payments for achieving measurable and continuous quality improvements.
Patient-Centered Oncology Payment (PCOP). Patient-Centered Oncology Payment (PCOP) is a family of alternative payment models developed by the American Society of Clinical Oncology to support higher quality, more affordable care for cancer patients, including “oncology medical home” services.
The basic PCOP payment model has two key elements that differ from current payment systems for oncology:
- An oncology practice could receive payments for four additional billing codes for payments to support services not covered by existing billing codes:
- New Patient Treatment Planning (a $750 payment for each patient);
- Care Management During Treatment (a $200 payment each month for each patient);
- Care Management During Active Monitoring (a $50 payment each month for each patient during treatment holidays and for up to six months following the end of treatment); and
- Participation in Clinical Trials (a $100 per month payment for each patient while treatment is underway and for six months afterward for trials in which practice support is not available).
- The payments for the additional billing codes would be adjusted based on the oncology practice’s performance in four areas:
- Avoiding emergency department visits and hospital admissions for complications of cancer treatment;
- Following evidence-based guidelines for the appropriate use of drugs, laboratory testing, and imaging studies, and using lower-cost drugs, tests, and imaging where evidence shows they are equivalent to higher-cost treatments and tests;
- Following evidence-based guidelines for high quality care near the end of a patient’s life;
- Providing care consistent with standards of quality defined by ASCO.
Two optional versions of PCOP bundle the new billing codes with existing billing codes and payments for other services:
- Consolidated Payments for Oncology Practice Services replaces the existing E&M and infusion payments the practice is receiving with three new sets of bundled billing codes (New Patient Payment, several levels of Treatment Month Payment, and several levels of Active Monitoring Month Payment),
- Virtual Budgets for Oncology Care defines virtual monthly budgets that cover not only the services delivered by the oncology practice but one or more other categories of services, such as hospital admissions, laboratory tests, imaging studies, and/or drugs.
Patient Education. Patient education helps people make informed decisions about their personal health-related behavior. It aims to improve health by encouraging compliance with medical treatment regimens and by promoting healthy lifestyles.
Asking patients to make behavioral changes is a complicated process. But making patient education materials available electronically — where and when it is needed — removes a barrier and helps patients learn what they need to do to maintain their health and prevent future health issues. The Patient Engagement Playbook includes resources to help patients manage their health and their care.
Patient Generated Health Data (PGHD). PGHD includes health-related data created, recorded, or gathered by or from patients, family members, or other caregivers outside of the clinical setting to help address a health concern. Historically, clinicians had limited access to their patients’ health data. They relied on information, like self-reported lifestyle habits and family health histories, collected during patient visits. The recent proliferation of consumer health technologies, such as online questionnaires, mobile apps, and wearable devices, has increased the frequency, amount, and types of PGHD available. These advances can enable patients and their caregivers to independently and seamlessly capture and share their health data electronically with clinicians and researchers from any location.
Health IT transforms our ability to collect accurate, reliable patient data. Using consumer apps and other technology, patients can track their health. Their mobile phones and computers are teeming with information on their diet, exercise habits, and vital signs. The wealth of information presents a new challenge — how to harness the data to improve clinical care and patient health.
Patient Portal. A patient portal is a secure website where patients can access their medical history and other health information. Using the portal, patients can typically complete forms online, communicate with clinicians, request prescription refills, pay bills, review lab results, and schedule appointments.
A PHR helps individuals manage their health information and engage actively in their healthcare.
Patient-Reported Outcome (PRO). A Patient-Reported Outcome is a measure of a patient’s health status or ability to function for which the data are collected and reported primarily or exclusively by the patient, not by a physician or other healthcare clinician. The patient’s report may be obtained by a healthcare clinician for use in a payment model, but the information in the report is generated by the patient, not through measurements made by the clinician.
Payer. A payer is a generic term used to describe an organization that transfers funds to a clinician to compensate it for the delivery of healthcare services. A payer transfers funds directly to the clinician rather than through an intermediary. For example, health insurance companies are payers, and self-pay patients are also payers.
Payer vs. Purchaser. In traditional health insurance arrangements, the purchaser is the individual or organization that pays premiums for a health insurance policy, and the payer is the health insurance company that pays claims under the policy. Self-insured employers are purchasers, but they are not typically payers, since they will usually engage a Third-Party Administrator to actually pay claims from clinicians. However, in some direct contracting arrangements between employers and clinicians, the self-insured employer may be both a purchaser and a payer. The distinction between purchasers and payers is important for many reasons:
- All else being equal, when three entities are involved – a purchaser, a payer, and a clinician – spending associated with healthcare services will be higher because of the administrative costs incurred by all three entities to manage their respective relationships.
- If a clinician reduces costs and accepts lower payments from a payer, the savings from those payments may or may not be passed on to the purchaser depending on the nature of the relationship between the purchaser and payer. For example, the premiums paid to a payer by a fully-insured purchaser may not decrease even if clinicians are paid less by the payer, whereas the savings from lower payments to clinicians will be passed on to self-insured purchasers.
- A payer may have financial reserves to cover random variation in spending on healthcare services that a purchaser does not.
Pay-for-Performance (P4P). In a pay-for-performance payment model, the amount that a clinician is paid for its services is changed in some way based on one or more aspects of the clinician’s performance. For example, in a pay-for-performance system intended to encourage higher-quality care, clinicians with higher scores on one or more measures of quality may receive higher fees than other clinicians.
A pay-for-performance system can provide rewards (either increases in payments for individual services or lump-sum bonus payments), penalties (such as reductions in payments for services), or both. A bonus or penalty can be either retrospective (a bonus is paid or a penalty is imposed at the end of a performance period) or prospective (future payments to the clinician are higher or lower based on performance in a prior period). Some P4P systems with retrospective penalties avoid the need to collect penalties from clinicians by imposing a “withhold” on the clinician’s payments at the beginning of the performance year; a clinician with good performance then receives both the withhold amount and a bonus payment and a clinician with poor performance forfeits the withhold. In some P4P systems, payments for all clinicians are simply reduced across the board and then some clinicians are given increased payments based on performance; in these systems, the net effect on an individual clinician depends on the size of the initial reduction and the size of the increases. For example, the Medicare Hospital Value-Based Purchasing Program reduces all payments to hospitals and then hospitals receive performance- based payment increases that may be more or less than the amount by which their payment was reduced.
A pay-for-performance system can be designed to reward or penalize absolute achievement (i.e., performance relative to a fixed achievement threshold), relative achievement (i.e., performance relative to other clinicians), improvement (i.e., the clinician’s current performance relative to its own performance in an earlier, baseline period), or some combination of the three.
In a pure pay-for-performance system, there is no change in the basic method by which the clinician is paid for services delivered. Services that can currently be billed for payment can continue to be billed and paid at the same payment rates, and services that cannot be billed for payment still cannot be billed or paid directly. In a retrospective P4P model, any additional payment awarded for high performance is paid after the services that resulted in the high performance have already been delivered. This means that if the clinician has to deliver services that are not paid for directly in order to achieve the high-performance level, they will have to have a way of paying for those services until the pay-for-performance bonus is paid, and the bonus payment may or may not be sufficient to cover those costs. In some payment models, a pay-for-performance program is combined with other payment changes, such as use of medical home payments, in order to give clinicians additional resources to deliver additional or different services than they do today but also encourage them to do so in ways that achieve higher performance on one or more measures of quality or spending.
For additional information, see Performance Period, Performance Score, Performance Standard, Performance Threshold, and Withhold.
Pay for Achievement. Pay for achievement is a form of pay-for performance in which rewards or penalties are based on the extent to which a clinician’s performance reaches a specified performance standard.
Pay for Improvement. Pay for improvement is a form of pay-for-performance in which rewards or penalties are based on the extent to which a clinician’s performance is better than it was in an earlier period of time.
Tournament Pay for Performance. A pay-for-performance model that rewards or penalizes a clinician based on how its performance compares to how other clinicians performed during the same performance period is sometimes referred to as “tournament” pay for performance, since a clinician does not know in advance what performance level will be viewed as high or low, and whether it “wins” or “loses” (in terms of bonuses or penalties) will depend on how other clinicians perform. Tournament models can discourage clinicians from sharing information on how to improve care because a clinician is more likely to receive higher payments if other clinicians perform poorly.
Pay for Reporting. In a pay for reporting system, a clinician’s payments are modified based on whether they report certain kinds of information to the payer (e.g., quality measures), but the payments are not modified based on the actual performance on those measures. Some payers have used pay for reporting systems as a first step in moving to a pay-for-performance system, since it is difficult to establish performance benchmarks in a P4P system without having baseline data on how clinicians perform on the measures that are going to be used.
Payment Model. A “payment model” is a description of a method for paying clinicians for healthcare services. A payment model defines methodologies for determining payment amounts rather than the exact amounts that will be paid to specific clinicians for specific patients. A payment model is typically implemented through a contract between a payer and a clinician that may include additional specifications regarding the patients who will receive services covered by the payment model, the parameters that will be used to convert the methodologies of the payment model into actual payment amounts, etc.
A payment model has four fundamental elements or building blocks:
- A definition of the services that will be covered by a single payment and the level of flexibility that the clinician has in determining which services can be delivered;
- The mechanism(s), if any, for controlling utilization and spending;
- The mechanism(s), if any, for ensuring good quality and outcomes; and
- The mechanism(s) for ensuring adequacy of payment.
There are multiple ways that each of these building blocks can be structured, and some approaches to payment may address multiple building blocks simultaneously. For example, “bundling” payments can both provide greater flexibility for a clinician in choosing the specific services to be delivered and can provide a mechanism for controlling utilization and spending on the services included in the bundle.
Payment System. A payment system is a payment model that has been implemented by a payer and is being used to pay clinicians for services.
Payment Update. A payment update is a change in the dollar amount of payments under a payment model to reflect changes in the costs of delivering services over time.
PBPM. PBPM is an abbreviation for Per Beneficiary Per Month, which is a term used in the Medicare program that means the same thing as Per Member Per Month (PMPM) in commercial insurance.
PBPY. PBPY is an abbreviation for Per Beneficiary Per Year.
PCOP. See Patient-Centered Oncology Payment.
PDL. PDL is an abbreviation for Preferred Drug List. See Formulary for more information.
Per Diem. A per diem payment is a payment that is made for each calendar day on which services are provided to a particular patient. For example, if a payer pays a hospital on a per diem basis, the total payment to the hospital for an individual patient would depend on how many days the patient spent in the hospital before being discharged, but not on how many services were delivered on any of those days. The amount of the per diem payment need not be the same for all days and all patients. For example, Medicare pays Inpatient Psychiatric Facilities on a per diem basis (see Inpatient Psychiatric Facility Prospective Payment System), but the per diem payments are higher for earlier days in a patient’s stay than for later days, and the per diem payment on any day varies from patient to patient based on the characteristics of the patient.
Performance Period. A period of time during which a clinician’s performance on quality or cost measures is calculated. In many payment models, the clinician’s performance during the performance period is compared to performance during a Baseline Period to determine whether improvements have occurred.
Performance Score. In many payment models, a clinician’s performance is evaluated based on multiple measures of quality or spending. Rather than making separate adjustments to payment based on the clinician’s performance on each individual measure, a performance score may be defined by multiplying the performance levels on each measure by a measure weight and then summing the products to calculate a single performance score that is then used to modify payment.
Performance Standard. A performance standard is a term generally used to describe a minimum level of performance that must be achieved by a clinician in order to participate in a payment model or to continue participating in the payment model.
Performance Threshold. A performance threshold is a term generally used to describe a level of performance which must be reached by a clinician in order to qualify for an increase in payment or to avoid a payment reduction.
Performance Year. See Performance Period.
Per Member Per Month Payment (PMPM). A “per member per month” payment is a form of capitation payment that is made to a healthcare clinician each month for each of the members of a health insurance plan who are assigned or attributed to that clinician. The key characteristic of the PMPM payment is that it does not vary based on how many services a particular patient receives. The size and purpose of the payment can vary dramatically, and the payment can be made in addition to service-based payments or it can be paid in place of service-based payments (i.e., a clinician would receive a PMPM payment and no longer be able to bill for one or more other types of services). Payments are generally made monthly because the membership of a particular health plan can change frequently and to also allow individuals to change clinicians. A PMPY – Per Member Per Year – payment is similar, but the payment covers services delivered over a 12-month period or a calendar year rather than services for a single month.
Personal Health Record (PHR). A PHR is an electronic application that people use to maintain and manage their health information in a secure and confidential environment. PHRs:
- Can include data from a variety of sources
- Remain separate from, and do not replace, the legal (electronic) medical record
- Can help people collect, store, and monitor their health information
A PHR helps individuals manage their health information and engage actively in their health and their care.
PFS. See Physician Fee Schedule.
PHO. See Physician-Hospital Organization.
Physician Fee Schedule (PFS). The Physician Fee Schedule is the system Medicare uses to pay physicians. In the PFS, the RVU weights assigned to CPT codes through the Resource Based Relative Value System (RBRVS) are multiplied by Geographic Practice Cost Indices specific to the community where a physician practices and by an overall national Conversion Factor in order to establish the dollar amounts that Medicare will pay for the delivery of the services defined by the CPT codes. Additional adjustments are made depending on whether the service is being delivered by a physician or other health professional, whether the physician is a Participating Physician, whether the services is delivered in a Health Professional Shortage Area (HPSA), and whether any special adjustments have been created for specific clinicians (such as primary care clinicians). Medicare will also pay for certain services that are not included in CPT codes by using HCPCS Level II codes. CMS assigns payment amounts to HCPCS Level II codes using various methods; for example, payments for drugs (Jcodes) are established using the ASP+x% payment model.
Many private payers use the Medicare Physician Fee Schedule to set their own payment rates, but they may use a different Conversion Factor than Medicare. This is often done by simply defining the payer’s fee schedule as a percentage of the Medicare fee schedule, e.g., the payments are “120% of Medicare.”
Physician-Focused Payment Model Technical Advisory Committee. The Physician-Focused Payment Model Technical Advisory Committee is established by the Medicare Access and Chip Reauthorization Act (MACRA) to provide recommendations to the U.S. Secretary of Health and Human Services as to whether proposals for physician-focused payment models submitted by individuals and organizations to the Committee meet the criteria that will be established by the Secretary in regulations.
Physician-Hospital Organization (PHO). A Physician-Hospital Organization is an organizational mechanism that allows a hospital and one or more physician practices to each remain independent but to jointly manage payment contracts or share certain kinds of services.
Pioneer ACO. See Accountable Care Organization.
Population-Based Payment. The term “population-based payment” is a generic term used to describe a capitation payment that is paid for each individual in population of patients independent of the services they receive. A population-based payment may either be paid in addition to existing fee-for-service payments or in place of some or all of the fee-for-service payments. See Capitation for more information.
Population Health Management. Population health management describes an approach to care delivery that is designed to help the individuals in a defined population avoid illness as well as to treat their illnesses when they occur. For example, population health management services include proactive efforts to ensure individuals receive preventive screenings, and to help them improve their health, to help them manage chronic conditions effectively. The “population” whose health is managed is a group of individuals who are defined or selected in some way other than through them seeking services to address health problems, e.g., a population could be all of the employees of an employer, all of the residents of a community, or all of the members of a health insurance plan.
Post-Acute Care. Post-Acute Care is a general term describing healthcare services that are delivered to a patient following their discharge from a hospital or the completion of other acute care services, and that are related in some way to the condition that was treated or the procedure that was used as part of the acute care services. Post-acute care services may be delivered in an institution, such as a Skilled Nursing Facility, in the patient’s home, such as through Home Health Services, or in an ambulatory care setting such as a physician’s office.
PPO. See Preferred Clinician Organization.
P4P. See Pay for Performance.
PMPM. See Per Member Per Month Payment.
PMPY. PMPY is an abbreviation for “per member per year” payment. See Per Member Per Month Payment for more information.
Potentially Avoidable Complication. A Potentially Avoidable Complication is a problem experienced by a patient during treatment that could potentially have been avoided if care had been delivered in a different way. As part of its Evidence-Informed Case Rates (ECRs), the Healthcare Incentives Improvement Institute (HCI3) has developed specific definitions for the potentially avoidable complications associated with each of a range of conditions and procedures and it has developed computer software that can identify such complications from information in claims data. The rate of potentially avoidable complications can be used as a performance measure in pay-for-performance systems as well as a method of implementing a payment model with a warranty for such complications.
Potentially Preventable Event. A Potentially Preventable Event is a problem experienced by a patient or a service delivered by a healthcare clinician that could potentially have been prevented if care had been delivered in a different way. 3M Information Systems has developed detailed definitions for a series of different Potentially Preventable Events, including “Potentially Preventable (Initial) Hospital Admissions,” “Potentially Preventable Emergency Department Visits,” “Potentially Preventable Complications,” and “Potentially Preventable Readmissions.”
Pre-Authorization or Prior Authorization. Preauthorization or prior authorization is a process whereby a clinician must seek explicit approval from a payer before delivering a particular service to a patient in order to receive payment for delivering that service.
Predictive Modeling. A predictive modeling system is a mathematical algorithm that uses information about a patient’s characteristics to predict future spending or outcomes for the patient. The typical purpose of predictive modeling is to identify patients who are likely to have high spending or poor outcomes so that additional or different services can be targeted to those patients in an effort to reduce spending or improve outcomes. Many predictive modeling systems are simply a variant of a risk adjustment system.
Preferred Clinician. A preferred clinician is a clinician that a patient is encouraged to use because the services delivered by the clinician are of higher quality or lower cost than other clinicians.
Preferred Clinician Organization (PPO). A PPO is a type of health insurance plan in which patients have lower cost-sharing or fewer restrictions if they receive services from a network of “preferred clinicians” who have contracted with the plan. Typically, clinicians are expected to accept lower payments for services from the payer (i.e., they give the payer a discount) in order to be designated as “preferred clinicians.”
Present on Admission (POA) Indicator. The Present on Admission Indicator is a letter code entered onto a hospital billing form to indicate whether a particular diagnosis code entered on the billing form reflected a health condition that existed when the patient was admitted to the hospital or whether the condition developed after admission and during the course of the hospital stay. If the POA Indicator is not present, diagnosis codes for Hospital-Acquired Conditions (HACs) are excluded when determining the DRG payment level for a patient who has been hospitalized and the rate of HACs is compared to other hospitals to determine whether a payment penalty will be applied.
Primary Care. Primary care is the principal source of healthcare services for an individual, particularly preventive healthcare services. Most people will receive primary care from a physician or other clinician who specializes in primary care services, but some patients who have serious health problems may receive their primary care from a specialist.
Primary Care Medical Home. See Medical Home.
Procedure Code. A procedure code is a combination of letters and numbers used to uniquely identify a particular healthcare service for purposes of record-keeping and billing for payment. For purposes of payment, services performed by physicians and services performed in physician offices and hospital outpatient departments are coded using CPT and HCPCS codes; services performed by hospital staff during hospital inpatient stays are coded on claims forms using the ICD system. Because physicians and hospitals generally bill separately for their services, the exact same service delivered to the same patient will be coded one way on the physician’s claim form and a different way on the hospital’s claim form. There is not a one-to-one crosswalk between the two systems, in many cases, CPT codes are more detailed than ICD procedure codes, but there are also ICD procedure codes for services for which there is no corresponding CPT code. A third method of coding procedures called SNOMED-CT (Systematized Nomenclature for Medicine – Clinical Terms) is used in electronic health record systems.
Process Measure. A type of quality measure based on whether a clinician delivered a particular service or followed a particular process in delivering a service. A process measure indicates whether something was done, not what the outcome was.
PROMETHEUS Payment. PROMETHEUS is an acronym for “Clinician Payment Reform for Outcomes, Margins, Evidence, Transparency, Hassle-reduction, Excellence, Understandability, and Sustainability.” PROMETHEUS Payment was originally developed with support from the Robert Wood Johnson Foundation and is based on a series of Evidence-Informed Case Rates that are now being maintained by the Healthcare Incentives Improvement Institute (HCI3). For more information, see Evidence-Informed Case Rate.
Prospective Attribution. See Attribution.
Prospective Payment. Prospective payment is a generic term for a payment model in which the amount of payment for delivery of a particular service or care of a particular condition is defined prior to the delivery or the service or care of the condition and the amount of payment does not change depending on the actual cost of delivering the service or caring for the condition. In contrast, in a cost-based reimbursement system, the amount of payment is determined retrospectively after services are delivered based on the actual costs incurred in delivering the services. In the Medicare program, large hospitals are paid under the Inpatient Prospective Payment System, which is so named because it replaced the cost-based reimbursement system under which most hospitals had been paid prior to 1983. (Hospitals designated as Critical Access Hospitals are still paid through cost-based reimbursement.)
Prospective Payment vs. Bundled Payment. A prospective payment does not need to be a “bundled” payment; indeed, most fee for service payments are “prospective payments” because the payment amount for the service is defined in advance and does not change regardless of how much it costs a clinician to deliver the service. Even though a payment is “prospective” it is generally paid retrospectively, i.e., after the service is delivered. Moreover, depending on the nature of the prospective payment model, the amount of payment to the clinician may depend on what service or services were delivered and the characteristics of the patient who received them, so the exact payment amount may not be known prospectively, but the rules for determining the payment amount will be defined before the services are delivered. For example, in the Medicare Inpatient Prospective Payment System, the amount of payment a hospital receives for a patient is not determined until after the patient is discharged, since the payment is based on a Diagnosis Related Group (DRG) and the DRG is determined based on the diagnoses assigned and procedures performed during the hospital stay. See also Retrospective Reconciliation and Cost-Based Reimbursement.
Prospective Payment vs. Case Rate. A prospective payment model may or may not be a case rate system. Because the term “prospective payment” is most commonly known in conjunction with the Medicare Inpatient Prospective Payment System which pays hospitals based on a case rate system, “prospective payment” is often viewed as a synonym for a case rate. However, Medicare has different Prospective Payment Systems for other clinicians that do not use case rates; for example, the Inpatient Psychiatric Facility Prospective Payment System (IPF PPS) and the Skilled Nursing Facility Prospective Payment System (SNF PPS) pay IPFs and SNFs on a per diem basis.
Prospective Bundled Payment vs. Retrospective Reconciliation. In a prospective bundled payment, the clinician or other entity that receives the payment is responsible for paying any other clinicians who deliver services as part of the bundle from the prospective payment. In other words, the recipient of the prospective bundled payment becomes the payer for any other clinicians who deliver services in the bundle. In contrast, in a bundled payment with retrospective reconciliation, the clinicians of services within the bundle may be paid directly by a third-party payer under standard fee-for-service arrangements, and then after the payer’s total spending on services within the bundle is reconciled against the bundled payment amount, the entity that has agreed to accept the bundled payment either receives an additional payment from the payer (the Net Reconciliation Payment Amount) or the entity must make a payment to the payer.
Clinician. Under federal law, the term “clinician” means any individual or organization that furnishes, bills for, or is paid for healthcare services, including physicians, hospitals, skilled nursing facilities, home health agencies, etc. In some contexts, the word “clinician” is used more narrowly to describe individuals such as physicians and nurse practitioners who deliver healthcare services, not hospitals or other institutions.
Clinician-Owned Health Plan. A clinician-owned health plan is a health insurance company that is owned by a healthcare clinician. A clinician-owned health plan may offer health insurance products that primarily or exclusively require plan members to receive covered healthcare services from the clinician, or it may offer health insurance products that permit plan members to receive services from a broader network of clinicians. A clinician’s financial risk under any given payment model is lower in a contract with its own health plan than with a separate third-party payer, because any differences between the amounts of payments for services and the costs of those services will ultimately go to the clinician organization. However, if the clinician-owned health plan is selling insurance products in return for a fixed premium, the clinician is taking on more insurance risk through the health plan than it would under typical contracts with a separate health insurance company. A clinician-owned health plan also enables a clinician to enter into direct contracts with employers and other purchasers where the purchaser retains insurance risk and the clinician accepts performance risk.
Clinician-Sponsored Health Plan. A health plan that is owned or significantly controlled by one or more healthcare clinicians. See Clinician-Owned Health Plan.
Purchaser. Purchaser is a term used to describe an individual or organization that purchases health insurance or healthcare services on behalf of itself or individuals affiliated with it (e.g., its employees) using funds not derived from health insurance premiums or other payments specifically intended to cover the individual or organization’s spending on healthcare services. A purchaser may pay for healthcare services directly or through a third-party payer, such as a health insurance plan. For example, a self-insured employer is a purchaser, because the employer uses funds generated through its business operations to pay for healthcare services for its employees. The federal government’s Medicare program is a purchaser, because it uses general tax revenues to pay for a significant portion of services to Medicare beneficiaries. See Payer vs. Purchaser for the differences between payers and purchasers.
Back to top
Q
QE. See Qualified Entity.
Qualified Entity (QE). A Qualified Entity is an organization that is authorized by federal law to receive Medicare claims data and to use it for public reporting of performance measures about healthcare clinicians and for analysis of opportunities to improve healthcare quality and affordability.
Quality and Resource Use Reports (QRUR). CMS produces Quality and Resource Use Reports for physician practices to enable them to compare the quality measures and spending measures for their patients to the patients of other physician practices.
Quality Gate. A quality gate is a threshold level on one or more quality measures that a clinician must meet in order to receive a supplemental payment, such as a Shared Savings payment.
QRUR. See Quality and Resource Use Reports.
Back to top
R
RBRVS. See Resource Based Relative Value Scale.
Rebasing. Rebasing is a process by which a new baseline performance level is established. For example, in a shared savings payment contract between a payer and a clinician, savings may initially be calculated based on a comparison of spending in each performance year relative to spending in a baseline year that occurred just before the contract began. When the contract is up for renewal, the payer may want to reset the baseline spending level to the last year of the previous contract, and then calculate savings based on comparisons of spending in future years to the new baseline year. However, this means that the clinician would no longer receive credit for any savings that were generated between the original baseline year and the new baseline year.
Reconciliation. See Retrospective Reconciliation.
Reference Price. A reference price is a payment amount that a payer believes is sufficient to enable patients to obtain a particular service or bundle of services from at least one clinician. In a payment model that uses reference prices, the payer indicates that it will pay no more than the reference price for a particular service, but the patient can still receive the service from a clinician that charges more than the reference price by paying the clinician the difference between the reference price and the clinician’s charge (i.e., a balance billing amount). If the payer will only pay for the service at clinicians who agree to charge the reference price without balance billing, the payer has merely created a narrow network consisting of clinician who agree to be paid at or below the reference price amount.
Regional Health Improvement Collaborative. A Regional Health Improvement Collaborative is a non-profit multi-stakeholder organization that implements initiatives to improve the quality and affordability of healthcare services in a state or sub-state region. An RHIC does not deliver or pay for care, and it is governed by a multi-stakeholder group including balanced representation from purchasers, payers, clinicians, and patients.
Regression to the Mean. Regression to the mean describes the expectation that when a clinician’s performance on a measure of quality, utilization, or spending is affected by random variables beyond the clinician’s control, a higher-than-average score on the measure during one measurement period will likely be followed be a lower score in the subsequent measurement period, and a low score will likely be followed by a higher score, even if there is no change in the underlying processes used to deliver services that would affect the measure. A corollary of this is that if one clinician is measured to be better than another clinician in one performance period, their relative positions may be reversed in the subsequent period simply due to random variation, and not due to any conscious effort by the poorer-performing clinician to improve. Regression to the mean is a problem in shared savings payment models and pay-for-performance payment models because measures of savings and performance may reflect random variation as well as conscious action by clinicians to reduce spending or improve performance. Many shared savings payment models include minimum savings rate provisions in an effort to avoid making shared savings payments based on random variation. See Minimum Savings Rate and Minimum Loss Rate.
Reinsurance. Reinsurance is an insurance policy purchased by a payer or clinician to cover a portion of its risk under a health plan or payment model. The form of reinsurance commonly used in healthcare is Stop-Loss Insurance.
Reinsurer. A reinsurer is an insurance company that offers reinsurance policies.
Relative Value Scale Update Committee (RUC). The Relative Value Scale Update Committee (RUC) is a 29-member committee staffed by the American Medical Association (AMA) that makes recommendations to CMS regarding the Relative Value Unit (RVU) that should be assigned to a CPT code.
Relative Value Unit (RVU). A Relative Value Unit (RVU) is a number that is assigned to a particular service as part of the Resource Based Relative Value Scale (RBRVS) to measure the resources associated with delivering that service relative to other services. In the Medicare Physician Fee Schedule, the RVU for a service is multiplied by a conversion factor to determine the actual payment amount for the service.
Work RVU (wRVU). The Work RVU for a service is a measure of the relative amount of work required by a physician to deliver the service compared to other services. Physician work is defined as a combination of the time required to perform the service, the technical skills and physical effort involved, the mental effort and judgment required, and the psychological stress associated with concern about risk to the patient. In addition to its use in determining payments under the Physician Fee Schedule, many organizations who employ physicians use wRVUs to measure the relative workload of physicians in order to determine their compensation.
Practice Expense (PE) RVU. The Practice Expense RVU for a service is a measure of the relative expenses incurred by a physician practice when a physician delivers the service, other than the expenses for compensation to the physician and professional liability insurance costs.
Non-Facility Practice Expense RVU. The Non-Facility Practice Expense RVU is a measure of the expenses incurred by the practice when the physician performs the service in the practice’s own office and not in a hospital or other facility that charges a separate Facility Fee.
Facility Practice Expense RVU. The Facility Practice Expense RVU is a measure of the expenses incurred by the practice when the physician performs the service in a hospital or other facility, rather than in the physician’s own practice office.
Professional Liability Insurance (PLI) RVU. The Professional Liability Insurance RVU is a measure of the professional liability insurance costs associated with delivering a particular service.
Total RVU. The Total RVU is the sum of the Work RVU, the Practice Expense RVU, and the Professional Liability Insurance RVU. There are two Total RVU amounts, a Non-Facility Total RVU and a Facility RVU, depending on whether the service is performed in a facility that charges a Facility Fee or not. The Medicare payment for a service is based on the Total RVU multiplied by the Conversion Factor, after adjusting the individual RVUs using the applicable Geographic Practice Cost Indices.
Reserve. For a clinician, a reserve is a pool of funds that the clinician maintains in order to cover the costs of services if the total cost of the services exceeds the total amount of payments the clinician receives. For a payer, a reserve is a pool of funds that the payer maintains in order to pay for claims for services delivered by clinicians when the total premiums received for the insured members fall short of the cost of the claims for covered services delivered to those insured members.
Resource Based Relative Value Scale (RBRVS). The Resource Based Relative Value Scale payment system for physicians was phased into the Medicare program between 1992 and 1996 and replaced the Customary, Prevailing, and Reasonable (CPR) system. The RBRVS defines Relative Value Units (RVUs) for each of the services defined in CPT codes, and the RVUs are then multiplied by a conversion factor to determine the dollar amount Medicare will pay for the services under the Physician Fee Schedule. Many payers other than Medicare use the RBRVS to establish their payments for physician services, but other payers may use a different conversion factor to determine the dollar amount of payment for a service from the RVU for that service.
Resource Use. Resource use is a measure of the relative amount of resources needed to deliver a particular set of services to patients. A resource use measure is calculated by estimating the relative amount of resources needed to deliver a particular service compared to other services, multiplying the number of each type of service by the resource use measure for that service, and then totaling all of the products together. The “resource use” for an individual service may or may not be defined based on the cost to a clinician of delivering that service.
Resource Utilization Group (RUG). Resource Utilization Groups (RUGs) is a risk-adjustment system used to adjust Medicare per diem payments to Skilled Nursing Facilities based on the type and intensity of rehabilitation and other services delivered to the patient, the patient’s health conditions, and the patient’s ability to carry out activities of daily living. There are 66 RUGs to which patients can be assigned, each of which has a specific weight used to adjust the payment amount. See Skilled Nursing Facility Prospective Payment System (SNF PPS).
Retrospective Reconciliation. One way to implement a prospective payment model is to make preliminary payments to the clinician on some other basis, then sum the preliminary payments made, compare the total to the prospective payment amount, and make a transfer of funds (the Net Payment Reconciliation Amount) between the clinician and the payer so that the clinician has received only the prospective payment amount. This process is called “retrospective reconciliation,” since it reconciles the preliminary payments against the prospective payment amount so that the actual total payments to the clinician equal the prospective payment. For example, in order to implement a multi-clinician bundled payment or an episode payment, each clinician might continue to bill and be paid for services under the standard fee-for-service system, but then all of those payments would be totaled and compared to the prospective payment amount; if the total is less than the prospective payment, the difference would be paid to the clinicians, and if the total is greater than the prospective payment, the clinicians would have to refund the difference to the payer. (Alternatively, the payer could create a withhold on the clinician’s fee-for-service payments, and then return all or part of the withhold if the fee-for-service payments are below the prospective payment amount.)
Revenue Cycle. Revenue cycle is a term used by financial professionals in the healthcare industry to describe the complete process needed to prepare claims for payment for the services they deliver and obtain payment for those claims. Different payment models will affect the revenue cycle in different ways and changes in cash flow under different payment models can create financial advantages or disadvantages for a clinician beyond the nominal comparison between the amount of payment and the service costs. For example, in a typical shared savings program, there is no change in the basic payment model, so if a clinician begins delivering a new service for which there is no direct payment, the clinician’s costs will increase but there will be no immediate change in the clinician’s revenue, so the change in care delivery will reduce the clinician’s margins in the short run. If the delivery of the new service reduces overall spending and results in a shared savings payment, the shared savings payment will be received well after the service was delivered, so the clinician may incur financing costs during the time between when the costs were incurred and when the shared savings payment was ultimately received.
RHC. See Rural Health Clinic.
RHIC. See Regional Health Improvement Collaborative.
Risk (for Payers). A payer is taking risk when it accepts fixed premium payments for a group of members in return for an obligation to pay for services to those members that may require spending exceeding the total premium revenue received.
Risk (for Clinicians). In the context of payment models, a clinician is said to be taking “risk” if the clinician agrees to take responsibility for delivering or arranging for the delivery of healthcare services to one or more patients in return for payment and if the total payments for those healthcare services may differ from the total cost of delivering those healthcare services in ways that cannot be definitively determined in advance. Virtually any payment model other than cost-based reimbursement has some degree of risk. Even fee-for-service payment involves risk for clinicians, because the fee for each service is fixed in advance, but the time and cost required to deliver the services to a group of patients may be higher or lower than the revenues received from the fee-for-service payments.
Downside Risk. A clinician is said to have downside risk if the clinician could incur costs that are greater than the payments received.
Insurance Risk. Insurance risk describes the components of risk resulting from factors related to patient health status or other factors that are beyond the control of a clinician. For example, the risk that a clinician will have patients whose health problems are more serious than average is an insurance risk.
One-Sided Risk. “One-sided risk” means that the payment model gives the clinician either upside risk or downside risk, but not both. The term “one-sided risk” is typically being used to describe a payment model such as shared savings that only has “upside risk.” However, pay-for-performance systems that include only penalties and no bonuses are one-sided risk payment models that involve only downside risk.
Performance Risk. Performance risk describes the components of risk resulting from factors that are within the control of the clinician. For example, the risk that a clinician will cause a patient to be infected during treatment and the risk that a clinician will order unnecessary services during treatment are performance risks, since these are factors that could be controlled by the clinician, and under a bundled or warrantied payment system, they could cause a clinician’s costs to increase without corresponding increases in revenue.
Shared Risk. Shared risk is a generic term for a payment model in which a payer and clinician share responsibility in some way when the funds available for payment differ from the costs of delivering services.
Two-Sided Risk. Two-sided risk means that the payment model gives the clinician both upside risk and downside risk.
Upside Risk. A clinician is said to have upside risk if the clinician could receive payments for services that are more than the costs incurred, i.e., if the clinician could generate a (positive) margin for delivering those services, or if it could achieve a higher margin than it achieves today. The “risk” is simply the uncertainty the clinician has regarding whether there will be a margin and how large it will be.
Insurance Risk vs. Performance Risk. The definition of what is insurance risk and what is performance risk depends on which of the factors that can cause the costs of care to increase for particular patients can be controlled by a particular clinician and which cannot. In the short run, clinicians cannot prevent health problems from occurring, so the discovery of a health problem in a patient is an insurance risk. Conversely, a clinician can take steps to avoid errors or other problems that result in higher costs, so those are performance risks. For example, if a clinician is responsible for caring for the health problems of a group of patients within a global payment, and a higher than expected number of those patients are diagnosed with cancer, that is an insurance risk, because the cancer diagnosis likely could not have been prevented by the clinician, and a principal reason why people obtain health insurance is to protect them against the costs of unexpected, expensive health problems. However, if the clinician uses unnecessary drugs or unnecessarily expensive drugs to treat those cancers, that is a performance risk, because the clinician could have treated the cancers at lower cost without compromising the quality of care. If a clinician is managing a patient population over an extended period of time, some factors that would otherwise be considered insurance risk could be considered performance risks; for example, if patients are found to have advanced colon cancer that could have been detected and addressed earlier through appropriate colonoscopies, then the advanced colon cancer could be viewed as a performance risk for a clinician that had the opportunity to arrange for better colon cancer screening, and only the early-stage cancer would be a true insurance risk.
Risk Adjustment. Risk adjustment systems are used in payment models to avoid holding clinicians accountable for factors affecting performance levels or costs that they cannot control. (Other terms used to describe a concept similar to “risk adjustment” include “acuity adjustment,” “severity adjustment,” and “casemix adjustment.”) Risk adjustment systems are used in two different ways in payment models:
- a risk adjustment system may be used to increase or decrease the amount of payment for a service or bundle of services based on characteristics of the patient and other factors that are expected to require more or less spending for that patient.
- a risk adjustment system may be used to adjust one or more of the measures of performance on quality, utilization, or spending that are used to determine a clinician’s payment. Since patient characteristics and factors may affect different measures in different ways, multiple risk adjustment systems could be used for different measures.
There are a variety of different risk adjustment systems used in payment models. Some risk adjustment systems are focused on particular types of services; for example, Diagnosis Related Groups (DRGs) are designed to risk adjust payments for inpatient hospital admissions and Home Health Resource Groups (HHRGs) are designed to risk adjust payments for home health agency services. Other risk adjustment systems, such as Hierarchical Condition Categories (HCCs), Clinical Resource Groups (CRGs), and Adjusted Clinical Groups (ACGs) are designed to risk adjust total spending on a patient population. In some cases, individualized risk adjustment systems have been developed for specific procedures, conditions, or episodes of care.
Most risk adjustment systems are calibrated based on their ability to predict current levels of spending or clinician performance for a patient or group of patients, with no distinction among factors affecting spending or performance that a clinician can or cannot control. For example, a risk adjustment system will generally assign a higher risk score to a patient if the amount that is typically spent on that patient is higher, even if those patients did not actually need all of the services they received. Similarly, a risk adjustment system for a quality measure will assign a higher risk score to patients for whom clinicians generally have lower quality scores, even if the factors leading to the low quality scores could have been changed by the clinicians. Consequently, a risk adjustment system may be adjusting away factors that clinicians can control while leaving them at risk for factors they cannot control.
Claims-Based Risk Adjustment. A claims-based risk adjustment system is a risk adjustment system that is based only on data recorded on healthcare claims data. Various studies have shown that factors about patients that are not recorded on claims data, such as the patient’s functional status and access to community resources, can have a significant impact on spending and quality performance levels.
Clinical Category Risk Adjustment. In a clinical category risk adjustment system, individuals are classified into groups based on differences in characteristics that are viewed as affecting spending or other performance measures. For example, individuals with one chronic condition may be placed into a different category than individuals with multiple chronic conditions, since, all else being equal, individuals with multiple chronic conditions will require more healthcare services and have poorer outcomes than those with only one chronic condition. A clinical category will typically be defined based on multiple characteristics, which means that there could potentially be hundreds of different categories to which a patient could be assigned based on different combinations of those characteristics. Each category is then assigned a weight indicating how much higher or lower spending or some other performance measure is expected to be for patients in that category than for patients in other categories. For example, the Diagnosis Related Group (DRG) system used by Medicare and many other payers to pay for inpatient hospital care is a clinical category risk adjustment system.
Concurrent Risk Adjustment. In a concurrent risk adjustment system, the information used in determining a risk score for a patient or assigning a patient to a risk category can include information about changes in a patient’s characteristics that occurred during the time period in which spending or performance is being measured. For example, if a patient has just been diagnosed with cancer or has just broken a bone, that information can be used in a concurrent risk adjustment system to modify the payment for the patient, since all else being equal, a patient with cancer or a broken bone will need more healthcare services than a patient without those problems.
Prospective Risk Adjustment. In a prospective risk adjustment system, the information used in determining a risk score for a patient or assigning a patient to a risk category only includes information about a patient’s characteristics prior to the period for which payment is being made or performance is being measured. For example, if a patient has just been diagnosed with cancer or has just broken a bone, that information cannot be used in a prospective risk adjustment system until the following year (or whatever period of time is used to calculate risk scores) and the payment for the patient in the current year will be the same as it would have been if the patient had not been diagnosed with cancer or broken a bone, even though, all else being equal, a patient with cancer or a broken bone will need more healthcare services than a patient without those problems.
Regression-Based Risk-Adjustment. A regression-based risk adjustment system uses linear regression analysis to develop a formula for assigning risk scores to patients. The regression analysis chooses the patient characteristics and the weightings of those characteristics that are statistically best at predicting spending in the year for which the regression analysis was performed. Each patient is then assigned a risk score by measuring them on each of the characteristics selected by the regression model, multiplying those individual measures by the weights assigned in the regression analysis, and then adding the products together to create an overall score. For example, the Hierarchical Condition Category (HCC) risk adjustment system used in the Medicare program is a regression-based risk adjustment system.
Prospective Risk Adjustment vs. Concurrent Risk Adjustment. Concurrent risk adjustment systems are more likely to accurately predict spending and performance in caring for patients than prospective risk adjustment systems, because they can incorporate the most current information about the patient’s health conditions. However, concurrent risk adjustment systems make it more difficult to predict what will be spent (since all of the factors affecting risk scores are not known in advance), and concurrent systems are more likely to be affected by upcoding.
Regression-Based Risk Adjustment vs. Clinical Category Risk Adjustment. A regression-based risk adjustment system will base a patient’s risk score on factors and weightings that were statistically best at predicting spending (or whatever performance measure was being analyzed) even if clinical logic would suggest that different factors should be important or that factors should be weighted differently. Moreover, the risk scores in a regression-based risk adjustment are calculated using a primarily linear formula even if clinical logic would suggest a non-linear relationship between spending and the factors used to calculate the risk scores (or between the factors and whatever performance measure is being analyzed). A clinical category system does not require linear relationships among the factors and can more easily incorporate clinical logic in the selection and weighting of the factors, but the more factors that are used and the finer the distinctions that are made based on how patients score on the individual measures, the larger the number of clinical categories that must be defined.
Risk Corridor. A risk corridor in a payment model is a method of limiting the financial risk a clinician faces if a large number of patients need above-average numbers of services or if an unexpectedly large number of patients need expensive services. These situations could occur because of random variation in patient characteristics that are not captured effectively by a risk adjustment system, particularly for clinicians with relatively small number of patients, or because of non-random but unexpected factors, such as a significant increase in the price of an essential drug or medical device. A risk corridor can also be used to protect a payer against paying much more for care than it costs a clinician to deliver care if the clinician develops a much more efficient way of delivering care after a payment arrangement has been finalized.
A risk corridor has two elements: (1) a specific range of values for the difference between the payer’s payment and the clinician’s costs of delivering services in return for that payment, and (2) a formula for allocating the portion of the gap between payment and costs in that range between the payer and clinician. For example, the clinician and payer might agree that if the total cost of services for all of the patients being cared for under a particular treatment bundle, condition-based payment, or population-based payment exceeds 110 percent of the total payments that are made for all of those patients, the payer will make an additional payment to the clinician to cover all or part of the costs above the 110 percent threshold. (The payer and clinician could also agree that if the total cost turns out to be significantly lower than the total payments that are made, the clinician will return to the payer all or part of the payments that are made beyond a certain percentage above the costs incurred.)
A payment model can have multiple risk corridors, not just one. For example, one risk corridor might define how the payer and clinician will share excess costs if the costs are between 110% and 120% of payments, and a second risk corridor might define what will be done if costs are more than 120% of payments.
Risk Limit. A risk limit is a cap on how much risk a clinician accepts before additional payments are made to cover its costs. In many payment models, risk limits are implicit rather than explicit; for example, in the Medicare Inpatient Prospective Payment System, hospitals can receive an Outlier Payment to cover a portion of the costs of an unusually expensive patient. The cost threshold that triggers the Outlier Payment is, in effect, a Risk Limit for the hospital, since the hospital’s risk in accepting a fixed DRG payment for patients with varying needs is limited by the ability to obtain an Outlier Payment if costs reach a certain level.
Risk Score. A risk score is a numeric value assigned to a particular patient in a risk adjustment system that indicates the relative level of spending that will be required for that patient or the relative level of quality or outcomes that can be achieved in the delivery of care to that patient relative to other patients.
Risk Stratification. Risk stratification is a way of adjusting payments for differences in patient characteristics by assigning patients to two or more categories based on characteristics that influence the costs of care and then adjusting the payment for a particular patient based on the category to which the patient is assigned. Risk stratification can be done using either a regression-based risk adjustment system or a clinical category risk adjustment system. If a regression-based risk adjustment system is used, the stratification categories are defined based on ranges of risk scores; if a clinical category risk adjustment system is used, the categories defined in the system can serve as the stratification categories. For example, the DRG system used by Medicare and other payers to pay hospitals is a risk stratification system based on a clinical category risk adjustment system.
Risk Scores vs. Risk Stratification. In risk adjustment systems that use a risk score, the payment for the patient is adjusted up or down in proportion to the risk score. This presumes a linear relationship between the risk adjustment score and the payment, i.e., if one patient has a 50% higher score than another, the payment for the first patient would be 50% higher than the second patient. In a risk stratification system, the amount of adjustment to the payment is particular to the category to which the patient is assigned, and there need be no systematic relationship between the payment adjustment associated with one category and the payment adjustment associated with another category. A risk stratification system is easier to incorporate into standard billing and claims payment systems because a billing code can be defined for each patient category in the risk stratification system. However, this may require the creation of many billing codes if there are many different risk categories. Using a risk score requires the use of only one billing code, but then a special mechanism is needed to adjust the amount of payment for that code because claims payment systems are designed to pay the same amount to a clinician for each billing code.
Risk Corridor vs. Risk Adjustment vs. Outlier Payment. Risk adjustment, risk corridors, and outlier payments are different and complementary methods of controlling a clinician’s risk in accepting a specific amount of payment without knowing exactly how many services it will need to deliver or pay for. A payment model may need to use all three components in order to adequately separate insurance risk and performance risk.
- Risk adjustment is a mechanism of increasing payment to a clinician if it delivers care to patients who have particular characteristics that are expected to require additional services or more expensive services, regardless of whether they actually receive such services.
- An outlier payment is an additional payment made to a clinician when the cost of services actually received by an individual patient exceeds a certain threshold.
- A risk corridor defines circumstances in which a clinician will receive higher payments if the aggregate cost of services actually received by a group of patients exceeds a certain threshold. (The risk corridor may also define circumstances in which a clinician will receive lower payments or return money to the payer if a group of patients receive services whose aggregate cost is lower than a threshold.)
RUC. See Relative Value Scale Update Committee.
RUG. See Resource Utilization Group.
Rural Health Clinic (RHC). A Rural Health Clinic (RHC) is a medical clinic specifically designated as such based on its location in a non-urbanized area designated as having a shortage of health professionals. Medicare pays RHCs an “all-inclusive rate” (AIR) based on their costs, but there is a maximum payment per visit for RHCs that are not part of a small hospital.
RVU. See Relative Value Unit.
Back to top
S
S-Code. An S-Code is a subset of the Level II codes that CMS creates and maintains as part of the Healthcare Common Procedure Coding System (HCPCS). S-codes are created for procedures and professional services that have not been incorporated into the CPT coding system, and that private payers but not Medicare will pay for. Examples of S-Codes include:
- S0315: Disease management program; initial assessment and initiation into the program
- S0317: Disease management program; per diem
- S0353: Treatment planning and care coordination management for cancer; initial treatment
Section 1115A. Section 1115A of the Social Security Act was added as part of the Affordable Care Act to establish the Center for Medicare and Medicaid Innovation (CMMI) to test payment models “where there is evidence that the model addresses a defined population for which there are deficits in care leading to poor clinical outcomes or potentially avoidable expenditures,” with a focus on “models expected to reduce program costs while preserving or enhancing the quality of care received by individuals.” See Center for Medicare and Medicaid Innovation.
Section 1115 Waiver. A Section 1115 waiver is a waiver granted by CMS to a state under Section 1115 of the Social Security Act to allow it to spend Medicaid funds in different ways than what would otherwise be required.
Self-Funded Employer. A self-funded employer is a business that is self-insured for the healthcare services for which it has agreed to pay for its employees.
Self-Insured. An employer or other purchaser is said to be self-insured if it takes direct responsibility for paying claims for healthcare services for its employees or members rather than purchasing health insurance policies from a separate health insurance company for each employee as a way of paying for those services. The majority of individuals in the U.S. who have employer-sponsored health insurance are part of a self-insured plan. Most self-insured employers are not completely self-insured; in addition to maintaining some level of financial reserve to cover claims costs, they generally purchase stop-loss insurance to protect them against large claims expenses (see Stop-Loss). Also, most self-insured employers do not pay the claims themselves, but they hire a Third Party Administrator (TPA) to pay those claims (under what is known as an Administrative Services Only contract) and then the self-insured employer pays the TPA for the actual cost of the claims plus an administrative fee. The TPA may or may not be a company that also sells health insurance policies. See Fully-Insured for comparison.
Self-Pay. A self-pay patient pays a clinician for its entire charge for a service from the patient’s own funds, rather than relying on an insurance company or other third-party payer to pay for all or part of the clinician’s charge for the service. If the patient has a health insurance plan with a deductible, the patient may pay for a service out of the patient’s own funds, but the patient may only have to pay the payment amount that the insurance company has negotiated for that service from the clinician.
Shared Risk. See Risk.
Shared Savings. “Shared savings” generally describes a payment arrangement between a payer and a clinician in which the total amount of payment to the clinician for its services is related in some way to how much the payer is spending in aggregate on those services or on a broader set of services and how that aggregate spending compares to a benchmark. There are many different ways to define a shared savings program, but most shared savings programs fall into one of two categories:
- In the most common form of shared savings program, including the programs being implemented in the Medicare Shared Savings program, the payer determines the actual amount it spent during a period of time on healthcare services for a group of patients cared for by a particular clinician, compares that spending amount to an estimate of what the payer expected to have spent on those services to those patients, and if the actual spending is lower than the expected amount (i.e., the payer determines that it has achieved savings), the payer makes a supplemental payment to the clinician which is proportional to the amount of savings, i.e., the payer shares its savings with the clinician.
- In some programs that are called “shared savings,” a clinician is determined to qualify for a shared savings payment if the payer’s spending on its patients is lower than the payer’s spending on other clinicians’ patients, even if the clinician in question did not actually reduce spending below the level that would have been expected based on that clinician’s past performance. It would be more accurate to describe these programs as a “pay for performance program based on spending,” since the clinician is being paid based on the fact that its spending has been and continues to be lower than what is achieved by other clinicians, not based on achieving savings beyond the current or expected level of spending.
There are three basic components to a Shared Savings Program, each of which can be structured in many different ways.
- A definition of which services for which patients are included in the spending being analyzed. In many cases, spending is based on services for patients who are “attributed” to a particular clinician.
- A method of calculating a comparison spending level (the benchmark) for determining whether the amount of actual spending qualifies for an additional “shared savings” payment. The formula for setting a benchmark may involve trending a baseline spending level for the same clinician, comparing the clinician’s spending to other clinicians or communities, or a combination of the two.
- A formula for determining the amount of the shared savings payment to the clinician. For example, the formula may include a minimum savings rate, a quality gate, and other elements.
In a pure Shared Savings Program, there is no change in the basic method by which the clinician is paid for services delivered. Services that can currently be billed for payment can continue to be billed and paid at the same payment rates, and services that cannot be billed for payment still cannot be billed or paid directly. In some payment models, a Shared Savings Program is combined with other payment changes, such as use of medical home payments, in order to enable clinicians to deliver additional or different services than they do today but also encourage them to do so in ways that reduce total spending on their patients. In some Shared Savings Programs, a clinician that qualifies for a shared savings payment receives that payment by submitting claims for a billing code that it could not previously use, but this billing code is not intended to represent payment for a particular service.
SIM. See State Innovation Model.
Site-Neutral. A payment for a service is said to be site-neutral if the amount of payment does not differ based on the type of facility or site where the service is performed, e.g., the payment is the same whether the service is performed in a physician’s office or a hospital outpatient department.
Site-of-Service Differential. A site of service differential is a difference in the amount of payment for the same service depending on where the service is performed. In the Medicare program, if a service is performed by a physician in a hospital outpatient department, the hospital is paid under the Outpatient Prospective Payment System and the physician is paid under the Physician Fee Schedule (using the Facility payment rate), whereas if the same service can be performed in the physician’s office, there is only a payment to the physician under the Physician Fee Schedule (using the higher Non-Facility payment rate). (The payment to the hospital outpatient department is known as a Facility Fee and is billed separately from the physician’s fee for performing the service.) It is important to note that the payment to the physician may be higher if the service is performed in the physician’s office than in the hospital, but if the service is performed in the hospital, both the physician and the hospital are paid separately, and the combined payment is generally higher if the service is performed at the hospital than in the physician’s office. Consequently, determining the site -of-service differential requires comparing combinations of payments from two different payment models or fee schedules.
Shared Savings vs. Gain-Sharing. The term “gainsharing” is typically used to describe an arrangement between two or more clinicians for dividing any surplus or profits that are generated when clinicians’ cost of delivering services is less than the amount of payment. “Shared savings” is typically used to describe an arrangement in which a payer makes an additional payment to one or more clinicians if the payer spends less in total payments than it would have otherwise expected to spend. For example, suppose a hospital and surgeon change the way surgery is delivered so that the costs to the hospital are reduced (e.g., the surgeon decides to use less expensive medical devices during surgery) and more patients are able to recover from surgery at home rather than going to a skilled nursing facility after discharge. The standard payment to the hospital would not change because lower-cost medical devices are used, but the hospital’s costs would decrease, and the hospital could agree to make a gain-sharing payment to the physician from the additional profit margin the hospital would generate. In contrast, if the physician and hospital redesigned care delivery so that fewer patients used skilled nursing facilities or patients had shorter stays in skilled nursing facilities, the standard payments to the hospital and physician would not change so there would be no new opportunity for gainsharing between the hospital and physician, but the payer’s spending on skilled nursing facilities would decrease, and the payer could agree to make a shared savings payment to the hospital and/or physician using a portion of the savings the payer received.
Skilled Nursing Facility (SNF). A Skilled Nursing Facility is an institution that provides 24-hour nursing services and other medical services for patients who require nursing care but do not require inpatient hospitalization.
Skilled Nursing Facility Prospective Payment System (SNF PPS). The Skilled Nursing Facility Prospective Payment System (SNF PPS) is the system Medicare uses to pay Skilled Nursing Facilities (SNFs). Under this payment model, a SNF receives an additional payment for each day that a patient is in the SNF (i.e., a per diem payment). The daily payment amount is adjusted for geographic differences in costs to establish a base payment rate for each facility. The base payment rate is then adjusted for each patient based on differences in patient characteristics and the types of services delivered using Resource Utilization Groups (RUGs). Each day of care is assigned to one of 66 RUGs based on the type and intensity of rehabilitation and other services delivered to the patient, the patient’s health conditions, and the patient’s ability to carry out activities of daily living. Each RUG has a specific weight that is multiplied by the facility’s base payment rate to determine the payment amount for that patient on that day.
SNF. See Skilled Nursing Facility.
Sole Community Hospital. In the Medicare program, a sole community hospital is a hospital that meets one of a series of criteria based on its distance from other hospitals, the travel time to other hospitals, and the proportion of inpatient care it provides for the residents of the hospital’s service area. Payments for Sole Community Hospitals are based partially on the Inpatient Prospective Payment System and Outpatient Prospective Payment System, but special adjustments are made in the amounts of payments they receive.
Spending. See Cost.
Specialist. A Specialist is a physician who delivers services in a particular area of medicine and does not deliver primary care to patients other than those with a medical problem in the physician’s area of specialty.
Standardized Payment. Because Medicare payments to clinicians are adjusted based on geographic cost differences (see Geographic Adjustment Factor) and other factors that are unrelated to the type of service delivered, the total spending for one clinician or one community may differ from the total spending for another clinician or another community even though the same number and types of services are delivered by both. To eliminate these unrelated differences, Medicare spending measures are often calculated using a single standardized payment for each service rather than the actual payment amounts. A similar approach can be used in comparing spending by private payers, since private payers pay different amounts for the same service in different communities and when the services are delivered by different clinicians.
Stark Law. The federal Ethics in Patient Referrals Act, commonly known as the “Stark Law,” prohibits physicians from referring Medicare and Medicaid patients to entities such as hospitals with which the physicians have a financial relationship (i.e., an ownership interest or a compensation arrangement) for the provision of “designated health services” except in a number of specifically exempt circumstances, e.g. where the physician is an employee of the entity, or for services meeting the In-Office Ancillary Services Exemption. In addition to the federal law, a number of states have enacted laws or regulations that also prohibit some types of self-referrals, including for services reimbursable by private health plans.
The Stark law and similar state self-referral statutes or regulations are intended to avoid having financial considerations influence physicians’ referral decisions. However, under a system that bundles payments to physicians and hospitals (or to physicians and other types of entities) to enable and encourage the delivery of coordinated services, physicians will inherently need to refer their patients to the clinician with which they have the bundled payment arrangement, and this may violate state and/or federal selfreferral laws or regulations. Moreover, because the laws or regulations typically have exemptions for employment arrangements, they can create a disadvantage for organizational structures in which physicians are independent compared to health systems that employ physicians.
For more information, see Fraud and Abuse Laws.
State Action Exemption. Under the “state action” doctrine of antitrust law, a state can encourage and facilitate joint efforts by healthcare payers (e.g., aligning payment methods and amounts) and joint efforts by clinicians (e.g., forming an Accountable Care Organization) without antitrust liability if the state (1) has a clearly articulated state policy supporting the need for common approaches, and (2) engages in active supervision of the activities that might otherwise cause antitrust concerns.
State Innovation Model (SIM). The State Innovation Models (SIM) Initiative is a program operated by the Center for Medicare and Medicaid Innovation that provides grants and technical assistance to state governments to facilitate planning and implementation of multi-payer payment reforms and delivery reforms in the state that will reduce costs and improve the quality of care for Medicare, Medicaid, and Children’s Health Insurance Program (CHIP) beneficiaries.
Step Therapy. A Step Therapy requirement in a health plan requires a clinician to treat a patient’s condition with a lower-cost therapy to determine whether it is effective before the health plan will cover the cost of a higher-cost therapy.
Stinting. Stinting means delivering fewer healthcare services than a patient needs to properly address their health problem(s).
Stop-Loss. A stop-loss is a provision in a payment contract that limits the amount that the clinician must spend on healthcare services, either for an individual patient or in aggregate for all patients. If costs exceed the threshold for triggering the stop-loss provision (referred to as the attachment point), the clinician will receive an additional payment from the payer to cover all or part of those costs.
Stop-loss insurance is a form of reinsurance that protects a clinician against unexpectedly high costs of delivering services by making a stop-loss payment when costs exceed a stop-loss threshold. A clinician who accepts a bundled payment from a payer may wish to purchase stop-loss insurance to cover unexpectedly high costs of services or high numbers or costs of claims from the other clinicians. Self-insured purchasers also purchase stop-loss insurance to protect them from high claims costs.
Aggregate Stop-Loss. An Aggregate Stop-Loss provision or reinsurance policy provides for additional payment if the total cost of services for a group of patients exceeds a specific amount. For example, if the Aggregate Stop-Loss is 110% of payments, then the clinician will receive an additional payment if the total cost of services for all patients exceeds 110% of the total payments made for those patients. An Aggregate Stop-Loss provision/policy does not provide any additional payment to a clinician with individual patients requiring expensive services if a sufficient number of other patients require fewer or lower-cost services. An aggregate stop-loss provision is equivalent to a risk corridor.
Individual Stop-Loss. An Individual Stop-Loss provision or reinsurance policy provides for additional payment if the cost of services for an individual patient exceeds a specific amount (the “Attachment Point”). For example, if the Individual Stop-Loss is $100,000, then the clinician will receive an additional payment if the cost of services for an individual patient exceeds $100,000. An Individual Stop-Loss provision/policy does not provide any additional payment to a clinician with a large number of patients who need many expensive services if none of the patients individually costs more than the individual stop-loss level. An individual stop-loss provision is equivalent to an outlier payment.
Swing Bed. In a hospital, a “swing bed” can be used either for patients who need acute care inpatient services or for patients who need skilled nursing facility (SNF) services.
Back to top
T
TCOC. See Total Cost of Care.
Third-Party Administrator (TPA). A Third-Party Administrator is an organization that receives and pays claims on behalf of a self-funded employer or other self-insured purchaser, but does not take any direct risk related to the cost of those claims. The claims-processing and other services are delivered by the TPA under an Administrative Services Only (ASO) contract with the purchaser.
Tie-Breaker. In many attribution methodologies, a patient or service is attributed to the clinician based on which clinician was highest on a measure such as the number of visits with the patient, the number of services delivered, etc. If two clinicians each were highest on that measure, then a second measure – the tie-breaker – is used to determine which of the two clinicians will be selected for attribution. For example, if a patient had the same number of visits during the year with two different clinicians, then the tie-breaker might be to identify the clinician who had the most recent visit with the patient.
Tiered Cost-Sharing. In a tiered cost-sharing system, clinicians or services are divided into two or more groups (“tiers”) based on one or more measures of cost or quality. When a patient uses a clinician or receives a service, the patient’s cost-sharing will depend on the tier to which the clinician or service is assigned. For example, the patient might be required to pay a higher co-payment for seeing a physician with lower quality scores, or the patient might be required to pay a higher proportion of the cost of a drug that is more expensive or less effective than another drug.
Tiered Network. A tiered network is a network of clinicians in which the clinicians are divided into two or more tiers based on measures of cost or quality, and different cost-sharing requirements or other rules apply depending on which tier a clinician is in. In a tiered network, all clinicians are generally considered to be “in-network” but with different cost-sharing requirements. A narrow network is an extreme form of a tiered network in which there are two “tiers” – in-network clinicians and out-of-network clinicians – and there is a large difference in cost-sharing requirements and benefits between in-network and out-of-network clinicians.
Total Cost of Care. The term “Total Cost of Care” is used to refer to the total amount that is spent on healthcare services for a group of individuals by one or more payers. It is technically a measure of spending, since it represents the cost to the payers based on the amounts they pay for the services, which may be more or less than the actual costs incurred by the clinicians who deliver those services.
Total Per Capita Cost. The Total Per Capita Cost is a measure calculated by dividing a payer’s total spending on a group of patients by the number of individuals insured by the payer. Total Per Capita Cost for Medicare beneficiaries is a measure being used by Medicare in the Physician Value-Based Payment Modifier program.
Tournament Pay for Performance. See Pay-for-Performance.
TPA. See Third-Party Administrator.
Track 1 ACO. See Accountable Care Organization.
Track 2 ACO. See Accountable Care Organization.
Track 3 ACO. See Accountable Care Organization.
Treatment-Based Bundled Payment. A treatment-based bundled payment is a payment that is triggered by delivery of a particular type of treatment (e.g., surgery or chemotherapy) and involves multiple services related to that treatment. In contrast, condition-based payment is a payment that is triggered by the appearance or existence of a health problem.
Trend (noun). The trend in spending or premiums is the rate at which they have increased or decreased over a period of time.
Trend (verb). In many payment methodologies, a measure of spending calculated during a baseline time period is “trended” forward to estimate what the spending would be expected to be during a performance period if no changes are made in the way care is delivered. For example, if the average spending per person in a base year was $10,000, and if the average annual inflation in spending was expected to be 3% per year, the $10,000 baseline amount could be trended forward by 3% per year to estimate that spending five years later would be expected to be $11,593 per person. (If actual spending in the fifth year was lower than $11,593, it would indicate that “savings” were generated, even though the amount of spending would still be higher than it was in the base year.) There are many different methodologies that can be used to do the trending; for example, in the Medicare Shared Savings Program, CMS has trended baseline spending measures using a blend of the percentage growth in spending and the absolute growth in per-beneficiary spending.
Trigger. In order for a clinician to receive a payment, something must be done to “trigger” the receipt of the payment. In fee-for-service payment, the trigger is the delivery of a service – a clinician delivers a service for which a patient or payer has previously agreed they will pay, and then the clinician invoices the payer (by submitting a claim). In a capitation payment model, the payment is not based on specific services (indeed, the capitation payment may be paid even if no services are delivered at all), so the trigger is something that associates the patient with the clinician – typically a formal assignment of the patient to the clinician or a statistical rule attributing the patient to the clinician. In a condition-based payment model, the trigger is a combination of the presence of the condition and an indication that the clinician will be treating that condition.
Truncation. Truncation is a statistical process that takes the most extreme values in a distribution and limits them to a fixed, pre-determined amount. For example, in any group of patients with a particular condition, some patients may have unusual problems that require a large number of expensive services for that condition (“outlier patients”). If a clinician is given a fixed payment to pay for as many services as the patients need for the condition, the small number of patients requiring the large number of expensive services could cause losses for the clinician. This problem can be mitigated by requiring the clinician to only be responsible for the truncated spending on these patients, i.e., the clinician would pay up $100,000 of spending, and then the payer would pay for spending on the expensive patients above $100,000. The patient remains a high cost patient for the clinician, but not as high cost as the patient would have been without truncation. See also Exclusion and Winsorization.
Back to top
U
UB-04. The UB-04 is the standard form used for submitting claims to payers for payment of hospital services. Its content and design is maintained by the National Uniform Billing Committee. The UB-04 form is called a CMS-1450 form in the Medicare program.
UCR. See Usual, Customary, and Reasonable.
Underinsured. Individuals are frequently being described as “underinsured” if they have health insurance but the cost-sharing requirements in the benefit design are such that the patient cannot afford to pay the cost-sharing for necessary services.
Underuse. Underuse is the use of a particular service less often than is necessary or justified based on evidence about its effectiveness.
UPL. See Upper Payment Limit.
Upcoding. Upcoding is a term used to describe assigning a diagnosis code to a patient or using a billing code for a service that results in a higher payment for a clinician than the payment that would result from using an alternative diagnosis or billing code that would be appropriate for the patient or service. In cases where payments to a health plan are risk adjusted, such as in the Medicare Advantage program, upcoding of diagnosis codes by clinicians can result in higher payments to the health plan but not to the clinicians. Upcoding does not necessarily mean that the codes used are inaccurate or inappropriate; in many cases there are multiple codes that can be used for the same patient condition or service and there is ambiguity about which code is appropriate to use in specific circumstances. However, if the weight assigned to a service or a diagnosis in a payment or risk adjustment system was based on one pattern of coding, then the weights may no longer be accurate if the pattern of coding changes.
Update. See Payment Update.
Uplift. An “uplift” is an increase in the amount of payment for one or more services beyond the amount that would otherwise be paid. In some prospective pay-for-performance systems, a clinician who meets the performance criteria will receive an uplift in the payment rates for certain services, i.e., the clinician will receive a higher payment when they bill for those services.
Upper Payment Limit (UPL). In the Medicaid program, states have discretion as to the amount clinicians are paid, but the federal government will only share the costs of payments up to the Upper Payment Limit.
Upside-Only Shared Savings. See Shared Savings.
Usual, Customary, and Reasonable (UCR). The “Usual, Customary, and Reasonable” amount is the amount that healthcare clinicians in a particular geographic region routinely charge for the same service to self-pay patients. Many payers used the UCR payment system to pay physicians before the creation of the Resource Based Relative Value Scale (RBRVS).
Utilization (by Patient). Utilization by a patient is the number of times that the patient receives a particular service. For example, a patient who visits the emergency room frequently is said to have high utilization of emergency services.
Utilization vs. Resource Use vs. Spending. A Utilization measure for a clinician describes the total number of services that are delivered to or ordered for a group of patients by the clinician; it does not distinguish whether the individual services delivered or ordered by the clinician were more costly or higher-priced than those delivered by another clinician. A Resource Use measure describes the relative time and costs associated with the services delivered to or ordered for a group of patients, but it does not distinguish whether there are differences in the prices for services that had the same costs or required the same number of resources. A Spending measure describes the total amount paid by a payer for the services delivered to a group of patients; one clinician may have higher spending than another clinician but lower Resource Use if the first clinician is paid more for the same services than the second clinician or if the first clinician orders services from other clinicians who have higher prices than those from whom the second clinician orders services.
Utilization (by Clinician). Utilization by a clinician is a measure of the number of times the clinician delivers or orders a particular service for a group of patients. For example, a physician who orders imaging studies frequently is said to have high utilization of imaging studies.
Back to top
V
Value. In healthcare, the word “value” has been used for over two decades in the Relative Value Units (RVUs) defined in the Resource-Based Relative Value Scale (RBRVS) to establish payments for physicians. In RBRVS, “value” is defined as the costs of the resources required to provide a service, including the physician’s time and the complexity of the service as well as out-of-pocket expenses such as office rent, equipment costs, insurance costs, etc.
More recently, the term “value” is widely being used to describe the combined assessment of both the quality and cost of a healthcare service or group of services. Conceptually, a “high-value” service is one that has high quality and low cost. However, because quality and cost are measured on fundamentally different scales and different people will convert one to the other in different ways (i.e., some people will be willing to pay more for an increment of quality than others), value is inherently a relative and partially subjective concept. Although one can objectively say that a service is “higher value” than another service if the first service has higher quality and the same cost, or if it has the same quality and lower cost, a subjective judgment is required if one service has both higher quality and higher cost than another service. Because of this, value cannot be defined as “quality divided by cost” as many have suggested. For example, assume that Clinician 1 delivers cancer treatment to a group of patients at a total cost of $25,000 per patient and Clinician 2 delivers a different type of cancer treatment to patients with similar characteristics at a total cost of $50,000. The patients treated by Clinician 1 live an average of 5 years, and patients treated by Clinician 2 live an average of 8 years. Dividing the outcome by the cost shows that Clinician 1 delivers 10.4 weeks of life per thousand dollars of treatment, while Clinician 2 delivers only 8.3 weeks of life per thousand dollars of treatment. If one defines “value” as “outcomes/cost,” Clinician 1 would be the higher-value clinician, yet most people would likely say the opposite, since Clinician 2 gives people an average of three extra years of life at an additional cost of only $25,000. If the two clinicians had different survival rates at the same treatment cost, or the same survival rates at different costs, the ratio wouldn’t be needed to make the comparison, but when costs and outcomes both differ, the ratio is not very helpful in determining which clinician has higher “value.”
Value-Based Incentive Payment Adjustment. In the Medicare Hospital Value-Based Payment Program, the value- based incentive payment adjustment is a percentage amount assigned to each hospital in each year based on the hospital’s scores on a series of performance measures. The hospital’s payments are then adjusted up or down by the percentage in the value-based incentive payment adjustment.
Value-Based Insurance Design (VBID). The term Value- Based Insurance Design is used to describe provisions of a health insurance plan’s benefit design that are explicitly structured to encourage plan members to use higher quality services, lower cost services, or both or to encourage patient or clinician behaviors that lead to better outcomes. This may include elements such as reducing patient cost-sharing for services deemed to be of high value, eliminating coverage for services deemed to be of low value, or encouraging or requiring patients to use clinicians designated as Centers of Excellence for specific types of services.
Value-Based Payment Modifier. The Value-Based Payment Modifier is a program established by Congress to adjust the Medicare payment for a service delivered by a physician to a Medicare beneficiary based on measures of the quality of care and the cost of care delivered by the physician during a performance period.
Value-Based Payment. Value-based payment is a generic term used to describe a payment model where the amount of payment for a service depends in some way on the quality or cost of the service that is delivered. There is no accepted minimum standard as to how much the payment must vary or what type of value measure must be used, so some payment models have been described as “value-based” even though there is very little difference in the amount of payments based on differences in quality or cost.
Value-Based Purchasing. Value-Based Purchasing is a generic term used to indicate that a purchaser is contracting for healthcare services in ways that are designed to improve quality, reduce costs, or both. Value-Based Purchasing may include the use of some form of Value-Based Payment, but it also can include Value- Based Insurance Design, Narrow Networks, and other approaches.
Value Modifier. See Value-Based Payment Modifier.
VM. See Value-Based Payment Modifier.
Volume-Based Adjustment. A volume-based adjustment is a mechanism by which the amount of payment to a clinician explicitly differs based on the number of patients the clinician cares for or the number of services or procedures the clinician delivers. To the extent that clinicians incur fixed costs to deliver a particular service or to care for patients with a particular condition, the average cost of the service and the average cost per patient will be higher for a clinician that delivers fewer of the services or cares for fewer patients with the condition, so the payment amount per service or per patient will need to be higher in order to cover the total costs of delivering the service. For example, Medicare has used a Low-Volume Adjustment to increase payments to hospitals with small numbers of patients.
Back to top
W
Warrantied Payment. A warrantied payment is an agreement by a clinician to deliver the services needed to address one or more complications of treatment without billing for or receiving additional payment for those services. For example, a clinician accepting a warrantied payment for surgical infections might agree that it would cover the costs of any hospital readmissions required to address infections from the surgery without receiving any additional payment. A warranted payment is not an outcome guarantee, i.e., the clinician is not guaranteeing that the warrantied events will not occur, the clinician is merely agreeing that if one of those events does occur, there will be no additional payment for the services needed to address that event. Most warrantied payments will involve a “limited warranty,” i.e., they will define the specific circumstances in which the warranty applies and those in which it does not.
Weight. In a payment model, a weight is a value assigned to a payment category or payment code that defines how large or small the payment for patients or services in that category or code should be relative to payments for patients or services in other categories or code. The weight is then multiplied by a conversion factor to determine the actual dollar amount of payment for that service. For example, in the Medicare Inpatient Prospective Payment System, each MS-DRG category is assigned a weight based on the level of hospital services and spending that are expected for patients in that category. The weight is multiplied by a conversion factor to determine how much a hospital will receive in dollars for a patient classified in that MS-DRG category.
In a performance measurement or risk adjustment system that is used as part of a payment model, a weight is a value that is multiplied by a particular measure or risk adjustment factor in order to combine that measure or factor with other factors in determining an overall performance score or risk score. A measure or factor with higher weight will have a greater influence on the overall performance or risk score. Two different payment models may use the same payment categories or risk adjustment factors, but they may apply different weights to those categories or factors reflecting differences in expected costs, spending, or performance on the particular patients for whom they are paying or the particular services for which they are paying. If one payment model uses bundles that include more services than a second payment model, both systems may choose to risk adjust the payments using the same factors, but the risk adjustment weights will likely be different. For example, the Medicare Inpatient Prospective Payment System and Long-Term Care Hospital Prospective Payment System both use the same DRG categories, but different weights are assigned to the categories in each system to reflect the different costs expected for patients with similar characteristics depending on whether they are receiving acute inpatient care or long-term hospital care.
Winsorization. Winsorization is a statistical process that takes the most extreme values in a distribution and replaces them with smaller values that are “closer” to the average for the distribution, e.g., any values above the 99th percentile in a distribution are replaced by the exact value at the 99th percentile. For example, in any group of patients with a particular condition, some patients may have unusual problems that require a large number of expensive services for that condition (“outlier patients”). If a clinician is given a fixed payment to pay for as many services as the patients need for the condition, the small number of patients requiring the large number of expensive services could cause losses for the clinician. This problem can be mitigated by requiring the clinician to only be responsible for the Winsorized spending on these patients, i.e., the clinician would pay up to the amount of spending at the 99th percentile of the spending distribution for all patients, and then the payer would pay for spending on the expensive patients above the 99th percentile amount. The patient remains a high cost patient for the clinician, but not as high cost as the patient would have been without Winsorization. See also Truncation and Exclusion.
Withhold. In a pay-for-performance system that includes penalties for poor performance, a payer may reduce payments to the clinician during the performance period below what the clinician would otherwise expect to receive (the reduction is the “withhold” amount); the payer then makes a supplemental payment at the end of the performance period if the clinician’s performance met a performance threshold, and the supplemental payment may be less than, equal to, or greater than the withhold amount. The use of a withhold avoids requiring the clinician to make a penalty payment to the payer if the clinician’s performance is poor; the clinician simply receives less money because it forfeits all or part of the withhold.